BK101
Knowledge Base
Physical Health
 The human body is an incredible
complex machine.
Don't ever take your body for granted. Everyone must fully understand the
responsibilities of
maintaining a
strong and healthy body.
The human body is an incredible
complex machine.
Don't ever take your body for granted. Everyone must fully understand the
responsibilities of
maintaining a
strong and healthy body.
Learn to Ask Questions.
First Aid - Vitals - Baseline
Prevention is Worth a Pound of Cure
Prevention is to stop something bad from happening or arising by taking the necessary actions and preparations.
Precautions are measured actions that are taken in advance to protect oneself from impending danger, damage or injury. having good judgment and evaluations in avoiding harm or danger.
Cautious is being alert and aware of possible dangers or harm. To be on guard and to put up a defense. Showing careful forethought by planning for possible risks or errors.
Preventive Medicine consists of measures taken for disease prevention, as opposed to just disease treatment. Prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention. Prevention requires social learning and public service assistance so that people can be given the tools and resources that are needed to help people self manage the responsibilities of their physical and mental health. Cigarettes alone causes 5 Billion Dollars in Heath Care Treatments from diseases caused by smoking.
Preventive Healthcare consists of measures taken for disease prevention, as opposed to just disease treatment. What do you need to be healthy? Learn what being healthy is.
Universal Healthcare - Intervention - Self Defense - Preserve
Personalized Medicine - Personalized Nutrition - Evidence Based Medicine
Risk Assessment - Number Needed to Educate - Assurance - Insurance
Prevention Science is the application of a scientific methodology that seeks to prevent or moderate major human dysfunctions before they occur.
Preventive Maintenance - Examination - Chain Reactions
Prevention through Design is the concept of mitigating occupational hazards by designing them out.
Holistic - Do No Harm - Duty of Care - Posture
Prophylactic is any device or mechanism intended to prevent harmful consequences. A medicine which preserves or defends against disease. Serving to prevent or protect against an undesired effect, especially disease. Condom (safe sex).
Prevention is better than a Cure because it's better and easier to stop a problem or illness from happening than it is to stop it or correct it after it has started. Treatment without prevention is simply unsustainable. It's Cheaper to Prevent Diseases than it is to Treat Diseases. Don't just treat the symptoms, you need to treat the whole system and find the root of the problem. But try to explain that to people who profit from treating diseases instead of curing them. Important services need to be public, not privatized corporate monopolies who care about money more than people.
Pain - Physical Therapy - Diagnosis (Health Assessment) - Lab Work
Knowledge is the Best Medicine. Knowledge has the power to heal. The fountain of youth is knowledge. A High Quality education is the best insurance against illness. Let food be thy medicine and let information be thy prevention.
Telemedicine - Sensors - Mental Sickness - Lethargic (fatigue)
Medicine is the science and the practice of the diagnosis, treatment, and prevention of disease. Medicine is also something that treats or prevents or alleviates the symptoms of disease, like a tonic. Not Natural.
Physical Health Education
Health Education is a profession of educating people about health. Areas within this profession encompass environmental health, physical health, social health, emotional health, intellectual health, and spiritual health, as well as sexual and reproductive health education.
Food and Nutrition - Health Assessment - Disease Burden
Physical Education is an educational course related to maintaining the human body through physical exercises (i.e. calisthenics). It is taken during primary and secondary education and encourages psychomotor learning in a play or movement exploration setting to promote health. (also known as Phys Ed or PE).
Exercise Prescription refers to the specific plan of fitness-related activities that are designed for a specified purpose, which is often developed by a fitness or rehabilitation specialist for the client or patient. Due to the specific and unique needs and interests of the client/patient, the goal of exercise prescription should be focused on motivation and customization, thus making achieving goals more likely to become successful.
Fatigue - Sitting too Much - Physical Therapy - Medical Procedure
Physical Fitness is a state of health and well-being and, more specifically, the ability to perform aspects of sports, occupations and daily activities. Physical fitness is generally achieved through proper nutrition, moderate-vigorous physical exercise, and sufficient rest. Before the industrial revolution, fitness was defined as the capacity to carry out the day’s activities without undue fatigue. However, with automation and changes in lifestyles physical fitness is now considered a measure of the body's ability to function efficiently and effectively in work and leisure activities, to be healthy, to resist hypokinetic diseases, and to meet emergency situations. Fitness Testing.
Health is feeling good and strong in the body and mind, and being free from disease or pain. Health is the level of functional and metabolic efficiency of a living organism. In humans it is the ability of individuals or communities to adapt and self-manage when facing physical, mental, psychological and social changes with environment. A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity or weakness. Health is defined as homeostasis of the cellular ecology, and a state where there has not been an inordinate loss, reversible or irreversible, of the structural and/or functional reserves of the body.
Body Burden - Health Assessment - Wellness - Healthcare Info
Right to Health is the universal minimum standard of health to which all individuals are entitled. The concept of a right to health has been enumerated in international agreements which include the Universal Declaration of Human Rights, International Covenant on Economic, Social and Cultural Rights, and the Convention on the Rights of Persons with Disabilities. There is debate on the interpretation and application of the right to health due to considerations such as how health is defined, what minimum entitlements are encompassed in a right to health, and which institutions are responsible for ensuring a right to health.
Public Health is the science and art of preventing disease, prolonging life and promoting human health through organized efforts and informed choices of society, organizations, public and private, communities and individuals, epidemiology, biostatistics and health services are all relevant. Environmental health, community health, behavioral health, health economics, public policy, mental health and occupational safety, gender issues in health, sexual and reproductive health are other important subfields. Department of Health and Human Services.
Population Health has been defined as "the health outcomes of a group of individuals, including the distribution of such outcomes within the group". It is an approach to health that aims to improve the health of an entire human population.
Adolescent Health or youth health, is the range of approaches to preventing, detecting or treating young people’s health and well being. The term adolescent and young people are often used interchangeably, as are the terms Adolescent Health and Youth Health. Young people's health is often complex and requires a comprehensive, biopsychosocial approach.
Health Geography is the application of geographical information, perspectives, and methods to the study of health, disease, and health care.
Health Sciences are those sciences which focus on health, or health care, as core parts of their subject matter. Because these two subject matter relate to multiple academic disciplines, both STEM disciplines as well as emerging patient safety disciplines (such as social care research) are relevant to current health scientific knowledge. Health sciences knowledge bases are currently diverse, with intellectual foundations which are sometimes mutually-inconsistent. There is currently an existing bias in the field, towards high valuation of knowledge deriving from controlling views on human agency (as epitomized by the epistemological basis of Randomized Control Trial designs); compare this against the more naturalistic views on human agency taken by research based on Ethnography for example).
Patient Education is the process by which health professionals and others impart information to patients and their caregivers that will alter their health behaviors or improve their health status. The value of patient education can be summarized as follows: Improved understanding of medical condition, diagnosis, disease, or disability. Improved understanding of methods and means to manage multiple aspects of medical condition. Improved self-advocacy in deciding to act both independently from medical providers and in interdependence with them. Increased Compliance – Effective communication and patient education increases patient motivation to comply. Patient Outcomes – Patients more likely to respond well to their treatment plan – fewer complications. Informed Consent – Patients feel you've provided the information they need. Utilization – More effective use of medical services – fewer unnecessary phone calls and visits. Satisfaction and referrals – Patients more likely to stay with your practice and refer other patients. Risk Management – Lower risk of malpractice when patients have realistic expectations. The competencies of a health educator include the following: Incorporate a personal ethic in regards to social responsibilities and services towards others. Provide accurate, competent, and evidence-based care. Practice preventative health care. Focus on relationship-centered care with individuals and their families. Incorporate the multiple determinants of health when providing care. Be culturally sensitive and be open to a diverse society. Use technology appropriately and effectively. Be current in the field and continue to advance education. Food and Nutrition.
Peer Education is an approach to health promotion, in which community members are supported to promote health-enhancing change among their peers. Peer education is the teaching or sharing of health information, values and behavior in educating others who may share similar social backgrounds or life experiences. Rather than health professionals educating members of the public, the idea behind peer education is that ordinary lay people are in the best position to encourage healthy behavior to each other.
Peer Mentoring (social learning)
Health Communication is the study and practice of communicating promotional health information, such as in public health campaigns, health education, and between doctor and patient. The purpose of disseminating health information is to influence personal health choices by improving health literacy. Because effective health communication must be tailored for the audience and the situation, research into health communication seeks to refine communication strategies to inform people about ways to enhance health or to avoid specific health risks. Academically, health communication is a discipline within communication studies. Health communication may variously seek to: Increase audience knowledge and awareness of a health issue. Influence behaviors and attitudes towards a health issue. Demonstrate healthy practices. Demonstrate the benefits of behavior changes to public health outcomes. Advocate a position on a health issue or policy. Increase demand or support for health services. Argue against misconceptions about health.
Health Literacy is the ability to obtain, read, understand and use healthcare information to make appropriate health decisions and follow instructions for treatment. There are multiple definitions of health literacy, in part, because health literacy involves both the context (or setting) in which health literacy demands are made (e.g., health care, media, internet or fitness facility) and the skills that people bring to that situation (Rudd, Moeykens, & Colton, 1999). Studies reveal that only 12 percent of the adults in the U.S. have proficient health literacy. This means 77 million adults have basic or below basic health literacy. These individuals have difficulty with common health tasks including reading the label of a prescribed drug. Low health literacy reduces the success of treatment and increases the risk of medical error. Health literacy is essential to promote healthy individuals and communities.
Self-Regulation Theory is a system of conscious personal management that involves the process of guiding one's own thoughts, behaviors, and feelings to reach goals. Self-regulation consists of several stages, and individuals must function as contributors to their own motivation, behavior, and development within a network of reciprocally interacting influences.
Adherence in medicine describes the degree to which a patient correctly follows medical advice. Most commonly, it refers to medication or drug compliance, but it can also apply to other situations such as medical device use, self care, self-directed exercises, or therapy sessions. Both patient and health-care provider affect compliance, and a positive physician-patient relationship is the most important factor in improving compliance, The cost of prescription medication also plays a major role.
Health Action Process Approach refers to a replacement of health-compromising behaviors (such as sedentary behavior) by health-enhancing behaviors (such as physical exercise). To describe, predict, and explain such processes, theories or models are being developed. Health behavioural change theories are designed to examine a set of psychological constructs that jointly aim at explaining what motivates people to change and how they take preventive action.
Theory of Planned Behavior states that attitude toward behavior, subjective norms, and perceived behavioral control, together shape an individual's behavioral intentions and behaviors.
Health Belief Model developed to explain and predict health-related behaviors, particularly in regard to the uptake of health services. The health belief model suggests that people's beliefs about health problems, perceived benefits of action and barriers to action, and self-efficacy explain engagement (or lack of engagement) in health-promoting behavior. A stimulus, or cue to action, must also be present in order to trigger the health-promoting behavior.
Health Psychology is the study of psychological and behavioral processes in health, illness, and healthcare. It is concerned with understanding how psychological, behavioral, and cultural factors contribute to physical health and illness. Psychological factors can affect health directly. By understanding psychological factors that influence health, and constructively applying that knowledge, health psychologists can improve health by working directly with individual patients or indirectly in large-scale public health programs. For example, chronically occurring environmental stressors affecting the hypothalamic–pituitary–adrenal axis, cumulatively, can harm health. Behavioral factors can also affect a person's health. For example, certain behaviors can, over time, harm (smoking or consuming excessive amounts of alcohol) or enhance health (engaging in exercise). Health psychologists take a biopsychosocial approach. In other words, health psychologists understand health to be the product not only of biological processes (e.g., a virus, tumor, etc.) but also of psychological (e.g., thoughts and beliefs), behavioral (e.g., habits), and social processes (e.g., socioeconomic status and ethnicity). By understanding psychological factors that influence health, and constructively applying that knowledge, health psychologists can improve health by working directly with individual patients or indirectly in large-scale public health programs. In addition, health psychologists can help train other healthcare professionals (e.g., physicians and nurses) to take advantage of the knowledge the discipline has generated, when treating patients. Health psychologists work in a variety of settings: alongside other medical professionals in hospitals and clinics, in public health departments working on large-scale behavior change and health promotion programs, and in universities and medical schools where they teach and conduct research.
Physiological Homeostasis is the tendency of the body to maintain critical physiological parameters (e.g., blood glucose level, blood salinity, blood pressure, core body temperature) of its internal environment within specific ranges of values.
Social and Behavior Change Communication is to develop communication strategies to promote positive behaviors which are appropriate to their settings and there by solve world's most pressing health problems. This in turn provides a supportive environment which will enable people to initiate, sustain and maintain positive and desirable behavior outcomes.
Physicians Committee for Responsible Medicine is changing the way doctors treat chronic diseases such as diabetes, heart disease, obesity, and cancer. By putting prevention over pills, doctors are empowering their patients to take control of their own health because not all doctors can be trusted. Unnecessary Treatments - Fraud.
Compassion makes Doctors better at their jobs. When health care providers take the time to make human connections that help end suffering, patient outcomes improve and medical costs decrease. Among other benefits, compassion reduces pain, improves healing, lowers blood pressure and helps alleviate depression and anxiety. Overworked Doctors can decrease compassion and increase mistakes.
Transtheoretical Model assesses an individual's readiness to act on a new healthier behavior, and provides strategies, or processes of change to guide the individual through the stages of change to Action and Maintenance. It is composed of the following constructs: stages of change, processes of change, self-efficacy, decisional balance and temptations.
Sadly, too many people do not participate in maintaining their health or take responsibility for their health, mostly because of their own stubborn neglect. They refuse to take advice from doctors and refuse to take advice from other people who are trying to help them. They also refuse to try to make changes that would have positive benefits to their health and to their well being. They prefer to suffer from their own ignorance instead of doing what is right or what is needed. Some people would rather come up with stupid idioms that say very little than try to explain their illogical reasoning. Too many people don't like to learn or listen, but for some strange reason, people will listen to bad advice without ever doing any research or verifying the information. People don't learn and listen when they should, but for some strange reason, they will listen to the wrong things and learn the wrong things when they shouldn't. This is some crazy sh*t. Education needs to improve and so does the Media.
Salutogenesis describes an approach focusing on factors that support human health and well-being, rather than on factors that cause disease (pathogenesis).
Human Physiology is the entire structure of a human being and comprises a head, neck, trunk (which includes the thorax and abdomen), arms and hands, legs and feet. Every part of the body is composed of various types of cells, the fundamental unit of life.
I'm Not Sick But I'm Not Well! - Harvey Danger - Flagpole Sitta [1997] (youtube) - "An illness can sometimes heal us".
Healing - Recovery - Treatment
Healing is the process of the restoration of health from an unbalanced, diseased or damaged organism. Healing involves the repair of living tissue, organs and the biological system as a whole and resumption of normal functioning. It is the process by which the cells in the body regenerate and repair to reduce the size of a damaged or necrotic area and replace it with new living tissue.
Cure is the end of a medical condition that helps end a person's sufferings. It may also refer to the state of being healed, or cured or make healthy again.
Treatment is care provided to improve a situation, especially medical procedures or applications that are intended to relieve illness or injury. The management of someone or something. An extended communication (often interactive).
First Aid - Humanistic - Physical Therapy - Sickness - Disorder
Remedy is a therapy that cures a disease or relieves pain. The act of correcting an error or a fault to set straight or right.
Recover is to get over an illness or shock. To get something back so it can be used again.
Recovery is to return to an original state. Gradual healing through rest after a sickness or injury. The act of regaining or saving something lost or in danger of becoming lost. A slow recovery will always be better than no recovery at all.
Long Road to Recovery is the process of becoming healthy again after an illness or injury. The act or process of returning to a normal state after a period of difficulty. The return of something that has been lost or stolen.
Recovery Approach - Nurse you back to health is to Educate the Mind. Placebos.
Acute Care is a branch of secondary health care where a patient receives active but short-term treatment for a severe injury or episode of illness, an urgent medical condition, or during recovery from surgery. In medical terms, care for acute health conditions is the opposite from chronic care, or longer term care. Medical Case Management is a collaborative process that facilitates recommended treatment plans to assure the appropriate medical care is provided to disabled, ill or injured individuals. It is a role frequently overseen by patient advocates.
Respite is a temporary relief from harm or discomfort. The act of reprieving or postponing or holding back punishment. A pause for relaxation.
Quality of Life - Comfort - Care - Palliative Care - Elderly Care
Health Care is the maintenance or improvement of health via the prevention, diagnosis, treatment, recovery, or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals in allied health fields. Physicians and physician associates are a part of these health professionals. Dentistry, pharmacy, midwifery, nursing, medicine, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training and other health professions are all part of health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health. Disease Burden.
Preservation is the activity of protecting something from loss or danger. An occurrence of improvement by virtue of preventing loss, injury or other change. The condition of being. Food Preserving.
Transitional Care refers to the coordination and continuity of health care during a movement from one healthcare setting to either another or to home, called care transition, between health care practitioners and settings as their condition and care needs change during the course of a chronic or acute illness. Older adults who suffer from a variety of health conditions often need health care services in different settings to meet their many needs. For young people the focus is on moving successfully from child to adult health services.
Physical Therapy - Messages - Rehabilitate
Continuity of Health Care is to what degree the care is coherent and linked, in turn depending on the quality of information flow, interpersonal skills, and coordination of care. Information Continuity is the process by which information relevant to a patient's care is made available to both the patient and the provider at the right place and the right time, to facilitate ongoing health care management and continuity of care. It includes that information on prior events is used to give care that is appropriate to the patient's current circumstance. Continuity of personal relationships, recognizing that an ongoing relationship between patients and providers is the undergirding that connects care over time and bridges discontinuous events. Continuity of clinical management. To avoid misinterpretation, the type of continuity should be agreed to before any related discussions or planning begin. Seamless care refers to an optimal situation where there is continuity in the healthcare even in the presence of many transitions. Analysis of medical errors usually reveals the presence of many gaps in health continuity, yet only rarely do gaps produce accidents. Patient safety is increased by understanding and reinforcing health care providers' normal ability to bridge gaps.
Hospitals - Health Facilities
Hospital is a health care institution providing patient treatment with specialized medical and nursing staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, seniors' geriatric hospitals, and hospitals for dealing with specific medical needs such as psychiatric treatment in a psychiatric hospital and certain disease categories. Specialized hospitals can help reduce health care costs compared to general hospitals. Hospitals are classified as general, specialty, or government depending on the sources of income received. Compare Hospitals.
There are 100,000 ICU beds in America and 790,000 ordinary beds across the country. Pandemics.
Teaching Hospital or university hospital is a hospital or medical center that provides medical education and training to future and current health professionals and that is involved in medical research. Teaching hospitals are often affiliated with medical schools and work closely with medical students throughout their period of matriculation, and especially during their clerkship (internship) years. In most cases, teaching hospitals also offer Graduate Medical Education (GME)/ physician residency programs, where medical school graduates train under a supervising (attending) physician to assist with the coordination of care. In addition to offering medical education to medical students and physician residents, many teaching hospitals also serve as research institutes.
Clinic is a healthcare facility that is primarily focused on the care of outpatients. Clinics can be privately operated or publicly managed and funded. They typically cover the primary healthcare needs of populations in local communities, in contrast to larger hospitals which offer specialized treatments and admit inpatients for overnight stays. Most commonly, the English word clinic refers to a general medical practice, run by one or more general practitioners, but it can also mean a specialist clinic. Some clinics retain the name "clinic" even while growing into institutions as large as major hospitals or becoming associated with a hospital or medical school.
Health Facility is any location where healthcare is provided. Health facilities range from small clinics and doctor's offices to urgent care centers and large hospitals with elaborate emergency rooms and trauma centers. The number and quality of health facilities in a country or region is one common measure of that area's prosperity and quality of life. In many countries, health facilities are regulated to some extent by law; licensing by a regulatory agency is often required before a facility may open for business. Health facilities may be owned and operated by for-profit businesses, non-profit organizations, governments, and in some cases by individuals, with proportions varying by country. See also the recent review paper, which provides a comprehensive classification of health facilities from the location analysis perspective.
Ambulatory Care - Out-Patient - Telemedicine - House Calls
Field Hospital is a temporary hospital or mobile medical unit that takes care of casualties on-site before they can be safely transported to more permanent facilities. This term was initially used in military medicine (such as the Mobile Army Surgical Hospital or MASH), but it is inherited to be used in civil situations such as disasters and major incidents. A field hospital is a medical staff with a mobile medical kit and, often, a wide tent-like shelter (at times an inflatable structure in modern usage) so that it can be readily set up near the source of casualties. In an urban environment, the field hospital is often established in an easily accessible and highly visible building (such as a manor house, restaurant, school, and so on). In the case of an airborne structure, the mobile medical kit is often placed in a normalized container; the container itself is then used as shelter. A field hospital is generally larger than a temporary aid station but smaller than a permanent military hospital. International humanitarian law, such as the Geneva Conventions, include prohibitions on attacking doctors, ambulances, hospital ships, or field hospitals buildings displaying a Red Cross, a Red Crescent or other emblem related to the International Red Cross and Red Crescent Movement.
Mobile Hospital is a medical center or a small hospital with full medical equipment that can be moved and settled in a new place and situation swiftly in order to provide medical services to patients or wounded persons in critical conditions such as war or natural disasters. In fact, a mobile hospital is a modular in that unit that every part of it is on the wheel, so it can be moved to another place easily, although all the required space and necessary equipment are considered so it can be utilized in the minimum time. With mobile hospital, one can provide medical services to wounded soldiers or patients near the war zone or any other place before moving them to the permanent hospital. In the mobile hospital, depending on the patient's situation and definitive treatment, admitted to the hospital and after evaluating the condition sent to another health center.
Shipping Container Clinic is a type of shipping container architecture using intermodal containers (shipping containers) as the structural element of a medical clinic that can be easily deployed to remote regions of the world. Shipping containers are ideal because of their inherent strength, wide availability and relatively low cost. In addition, and most relevant, shipping containers can be deployed anywhere in the world with the clinic already assembled within the container. This means pop-up clinics can be operational within days after deployment.
Hospital Ship is a ship designated for primary function as a floating medical treatment facility or hospital. Most are operated by the military forces (mostly navies) of various countries, as they are intended to be used in or near war zones. In the nineteenth century redundant warships were used as moored hospitals for seamen. The Second Geneva Convention prohibits military attacks on hospital ships, though belligerent forces do have rights of inspection and may take injured enemy patients as prisoners of war.
Aid Station is a temporary facility (often a tent, table, or general rest area) established to provide supplies to endurance event participants or medical first aid and provisions during major events, disaster response situations, or military operations. Aid stations may be divided into sections where the station serves both medical and non-medical functions.
Doctor - Physician
Doctor or Physician is a professional who practices medicine, which is concerned with promoting, maintaining, or restoring health through the study, diagnosis, and treatment of disease, injury, and other physical and mental impairments. Physicians may focus their practice on certain disease categories, types of patients and methods of treatment—known as specialties—or they may assume responsibility for the provision of continuing and comprehensive medical care to individuals, families, and communities—known as general practice. Medical practice properly requires both a detailed knowledge of the academic disciplines (such as anatomy and physiology) underlying diseases and their treatment—the science of medicine—and also a decent competence in its applied practice—the art or craft of medicine. National Rural Health Association states that rural areas could be short 45,000 doctors by 2020. And other trade groups warn those numbers of unfilled positions could loom even larger. Since 2010, more than 70 rural hospitals have closed. Telemetry Systems.
Medicine is the science and practice of establishing the diagnosis, prognosis, treatment, and prevention of disease. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness. Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Residency or postgraduate training is a stage of graduate medical education and someone who practices medicine, usually in a hospital or clinic, under the direct or indirect supervision of a senior clinician registered in that specialty such as an attending physician or consultant. In many jurisdictions, successful completion of such training is a requirement in order to obtain an unrestricted license to practice medicine, and in particular a license to practice a chosen specialty. An individual engaged in such training may be referred to as a resident, house officer, registrar or trainee depending on the jurisdiction. Residency training may be followed by fellowship or sub-specialty training. Whereas medical school teaches physicians a broad range of medical knowledge, basic clinical skills, and supervised experience practicing medicine in a variety of fields, medical residency gives in-depth training within a specific branch of medicine. Internship in medicine means a physician in training who has completed medical school and has a medical degree, but does not yet have a full license to practice medicine unsupervised. On the Job Training.
Medical Education is education related to the practice of being a medical practitioner; either the initial training to become a physician (i.e., medical school and internship), or additional training thereafter (e.g., residency, fellowship and continuing medical education). Medical education and training varies considerably across the world. Various teaching methodologies have been utilised in medical education, which is an active area of educational research. Medical education is also the subject-didactic academic field of educating medical doctors at all levels, applying theories of pedagogy specifically in the context of medical education. Doctor of Medicine or M.D., is a medical degree, the meaning of which varies between different jurisdictions.
Nurse (care giving) - Medical Ethics - Duty of Care - Insurance
Early Historical Doctors: Herophilos Greek Physician 335–280 or 255 BC) - (Galen Greek Physician AD 129 – c.200/c.216) Galenic Corpus.
Health Care Provider is an individual who provides preventive, curative, promotional or rehabilitative health care services in a systematic way to people, families or communities. A health professional may operate within all branches of health care, including medicine, surgery, dentistry, midwifery, pharmacy, psychology, nursing or allied health professions. A health professional may also be a public/community health expert working for the common good of the society.
Compare Doctors (ratings)
The Global Standard (ICHOM) value-based health care focusing on health outcomes.
Bedside Manner or a good bedside manner is typically one that reassures and comforts the patient while remaining honest about a diagnosis. Vocal tones, body language, openness, presence, honesty, and concealment of attitude may all affect bedside manner. Poor bedside manner leaves the patient feeling unsatisfied, worried, frightened, or alone. Bedside manner becomes difficult when a healthcare professional must explain an unfavorable diagnosis to the patient, while keeping the patient from being alarmed.
Ethics in The Medical Industry (customized care) - Errors made by Doctors
Specialist in medicine is a branch of medical practice. After completing medical school, physicians or surgeons usually further their medical education in a specific specialty of medicine by completing a multiple year residency to become a medical specialist.
Medical Specialists (webmd) - More Specialties
Clinician is a health care professional that works as a care giver of a patient in a hospital, skilled nursing facility, clinic, or patient's home. Clinicians work directly with patients rather than in a laboratory or as a researcher. A clinician may diagnose, treat, and otherwise care for patients. For example, physicians, nurses, nurse practitioners, clinical pharmacists, physician assistants, speech-language pathologists (SLP), and speech-language pathology assistants (SLPA) are clinicians. Midwives can be considered clinicians, although some midwives may emphasize de-medicalizing giving birth. Many clinicians take comprehensive exams to be licensed and some complete graduate degrees (master's or doctorates) in their field of expertise. A main function of a clinician is to manage a sick person in order to cure the effects of their illness. The clinician can also consider the impact of illness upon the patient and his family as well as other social factors.
Board Certification is the process by which a physician or other professional in the United States demonstrates a mastery of basic knowledge and skills through written, practical, or simulator-based testing.
Accreditation (school degrees)
Medicine Categories (wiki) - Medicine Categories (wiki)
Medical Terminology is language used to precisely describe the human body including its components, processes, conditions affecting it, and procedures performed upon in. It is to be used in the field of medicine. Notable aspects of medical terminology include the use of Latin terms and regular morphology, with the same suffixes and prefixes use quite consistently for a particular meaning. This regular morphology means that once reasonable number of morphemes are learned it becomes easy to understand very precise terms build up from these morphemes. A lot of medical language is anatomical terminology, concerning itself with the names of various parts of the body. Medical Terms Definitions.
In Home Care - Visiting Doctors - Doctors making House Calls
Concierge Medicine is a relationship between a patient and a primary care physician in which the patient pays an annual fee or retainer. This may or may not be in addition to other charges. In exchange for the retainer, doctors agree to provide enhanced care, including principally a commitment to limit patient loads to ensure adequate time and availability for each patient. The practice has been referred to as concierge medicine, retainer medicine, membership medicine, cash-only practice, and direct care. While all "concierge" medicine practices share similarities, they vary widely in their structure, payment requirements, and form of operation. In particular, they differ in the level of service provided and the fee charged. Estimates of U.S. doctors practicing concierge medicine range from fewer than 800 to 5,000.
Direct Primary Care is a type of primary care billing and payment arrangement made between patients and medical providers, without sending claims to insurance providers. It is an umbrella term, incorporating various health care delivery systems that involve direct financial relationships between patients and health care providers.
Operation Safety Net is a Street Medicine program in Pittsburgh, Pennsylvania. OSN was founded when Dr. Jim Withers and Mike Sallows began to make "house calls" together at night under the bridges, along the river banks and in the abandoned buildings of Pittsburgh.
Mercy Atlanta everyone deserves exceptional medical care regardless of Insurance or income status.
One recent estimate cited in a legislative report on homelessness suggested that more than $60 million in medical costs for Atlanta's homeless population were passed on to taxpayers.
People who saw their doctor for acute pain later in the workday were more likely than those with morning appointments to get a prescription for opioid painkillers. The people with late-in-the-day appointments — or seen later than their scheduled appointment time — were more likely to leave with a prescription for opioid painkillers than those with early appointments. Another recent study suggests that patients seen later in the day are less likely to receive recommended cancer screening tests, like mammograms.
Doctors Without Borders - International Medical Corps - Fund Medical Treatments for People in Need.
Examinations - Diagnosis
Physical Examination is the process by which a medical professional investigates the body of a patient for signs of disease. It generally follows the taking of the medical history—an account of the symptoms as experienced by the patient. Together with the medical history, the physical examination aids in determining the correct diagnosis and devising the treatment plan. This data then becomes part of the medical record. Sensors - Imaging (EEG).
Examine is to consider in detail and subject to an analysis in order to discover essential features or meaning. Observe, check out, and look over carefully or inspect. Question thoroughly and closely. Put to the test, as for its quality, or give experimental use to.
Examination is the act of examining something closely for mistakes. A set of questions or exercises evaluating skill or knowledge. Formal systematic questioning and a detailed inspection. A Thorough Search.
Forensic Science - Evaluations - Assessments - Over Diagnosis.
Critique is a serious examination and judgment of something. Critical Thinking.
Diagnosis is the identification of the nature and cause of a certain phenomenon.
Medical Diagnosis is the process of determining which disease or condition explains a person's symptoms and signs.
Diagnosis of Exclusion is a diagnosis of a medical condition reached by a Process of Elimination, which may be necessary if presence cannot be established with complete confidence from history, examination or testing. Such elimination of other reasonable possibilities is a major component in performing a differential diagnosis. Troubleshoot - Reason by Deduction.
Diagnostic Test or Medical Test is a kind of medical procedure performed to detect, diagnose, or monitor diseases, disease processes, susceptibility, and determine a course of treatment. It is related to clinical chemistry and molecular diagnostics, and the procedures are typically performed in a medical laboratory.
Comprehensive Metabolic Panel is a panel of 14 Blood Tests which serves as an initial broad medical screening tool. The CMP provides a rough check of kidney function, liver function, diabetic and parathyroid status, and electrolyte and fluid balance, but this type of screening has its limitations. Abnormal values from a CMP are often the result of false positives and thus the CMP may need to be repeated (or a more specific test performed), requiring a second blood drawing procedure and possibly additional expense for the patient, even though no disease is present. This test is also known as SMA12+2 test. The CMP is an expanded version of the basic metabolic panel (BMP), which does not include liver tests. A CMP (or BMP) can be ordered as part of a routine physical examination, or may be used to monitor a patient with a chronic disease, such as diabetes mellitus or hypertension. Previous names for the panel of tests have been Chem 12, Chemistry panel, Chemistry screen, SMA 12, SMA 20 and SMAC (Sequential Multiple Analysis - Computer). The tests are performed on machines based on the AutoAnalyzer invented in 1957.
Smartphone Blood Test - Heart Info - Blood Work
Reference Range is the range of values for a physiologic measurement in healthy persons (for example, the amount of creatinine in the blood, or the partial pressure of oxygen). It is a basis for comparison (a frame of reference) for a physician or other health professional to interpret a set of test results for a particular patient. Some important reference ranges in medicine are reference ranges for blood tests and reference ranges for urine tests.
Baseline - Vitals - Remote Sensors
Medical Test is a medical procedure performed to detect, diagnose, or monitor diseases, disease processes, susceptibility, or to determine a course of treatment. Medical tests relate to clinical chemistry and molecular diagnostics, and are typically performed in a medical laboratory, which is a laboratory where tests are carried out on clinical specimens to obtain information about the health of a patient to aid in diagnosis, treatment, and prevention of disease.
Analytical Chemistry
In Vitro Diagnostics tests a sample of tissue or bodily fluids, such as: Liquid biopsy, Microbiological culturing, which determines the presence or absence of microbes in a sample from the body, and usually targeted at detecting pathogenic bacteria. Genetic testing, Blood Glucose testing, Liver function testing, Calcium testing, Testing for electrolytes in the blood, such as Sodium, Potassium, Creatinine, and Urea.
Rapid test could diagnose serious conditions within two hours. The project, named DIAMONDS (Diagnosis and Management of Febrile Illness using RNA Personalised Molecular Signature Diagnosis).
Biopsy is a medical test commonly performed by a surgeon, interventional radiologist, or an interventional cardiologist involving extraction of sample cells or tissues for examination to determine the presence or extent of a disease.
3D Optical Biopsies within reach thanks to advance in Light Field Technology. - Light Technology.
Triage is the process of determining the priority of patients' treatments based on the severity of their condition.
Prognosis is a medical term for predicting the likely outcome of one's current standing.
Autopsy is a highly specialized surgical procedure that consists of a thorough examination of a corpse by dissection to determine the cause and manner of death and to evaluate any disease or injury that may be present. It is usually performed by a specialized medical doctor called a pathologist. Also known as a post-mortem examination, obduction, necropsy, or autopsia cadaverum.
Condition is a state at a particular time. The state of either good health or physically fit or an illness, disease, or other medical problem. ('in condition' or 'in shape' or 'out of condition' or 'out of shape').
Medical History is information gained by a physician by asking specific questions with the aim of obtaining information useful in formulating a diagnosis and providing medical care to the patient. The patient or other people who know the person and can give suitable information. Medically relevant complaints reported by the patient or others familiar with the patient are referred to as symptoms, in contrast with clinical signs, which are ascertained by direct examination on the part of medical personnel. Most health encounters will result in some form of history being taken. Past medical history is any previous surgery or operations including major illnesses. The history requires that a clinician be skilled in asking appropriate and relevant questions that can provide them with some insight as to what the patient may be experiencing. The standardized format for the history starts with the chief concern (why is the patient in the clinic or hospital?) followed by the history of present illness (to characterize the nature of the symptom(s) or concern(s)), the past medical history, the past surgical history, the family history, the social history, their medications, their allergies, and a review of systems (where a comprehensive inquiry of symptoms potentially affecting the rest of the body is briefly performed to ensure nothing serious has been missed). After all of the important history questions have been asked, a focused physical exam (meaning one that only involves what is relevant to the chief concern) is usually done. Based on the information obtained from the H&P, lab and imaging tests are ordered and medical or surgical treatment is administered as necessary. Heteroanamnesis is a record of past events and circumstances that are or may be relevant to a patient's current state of health. Informally, an account of past diseases, injuries, treatments, and other strictly medical facts. Body Burden Test.
Personal Health Record is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions (such as hospitals) and contains data entered by clinicians (such as billing data) to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or (collected passively) from a smartphone.
Monitoring (telemedicine)
Point-of-Care Testing is defined as medical diagnostic testing at or near the point of care—that is, at the time and place of patient care. This contrasts with the historical pattern in which testing was wholly or mostly confined to the medical laboratory, which entailed sending off specimens away from the point of care and then waiting hours or days to learn the results, during which time care must continue without the desired information.
A Starving Mom Suddenly Ate 40 Cookies. This Is What Happened To Her Heart (youtube) - This video shows how correctly diagnosing people can be extremely difficult at times. Problem solving is a skill that everyone should master.
Chubbyemu is a youtube channel for Medical videos and telling stories in medicine. These are variations on cases I, or my colleagues, have seen in the past. The main goal of these videos are to tell a story about people, as we each have a unique story to tell.
Ai-Med mission to bring medicine into the Artificial Intelligence future.
SOCRATES is an acronym used to gain an insight into the patient's condition, and to allow the health care provider to develop a plan for dealing with it. Site – Where is the pain? Or the maximal site of the pain. Onset – When did the pain start, and was it sudden or gradual? Include also whether it is progressive or regressive. Character – What is the pain like? An ache? Stabbing?
Radiation – Does the pain radiate anywhere? Associations – Any other signs or symptoms associated with the pain? Time course – Does the pain follow any pattern? Exacerbating/relieving factors – Does anything change the pain? Severity – How bad is the pain?
OPQRST is a mnemonic acronym used by medical professionals to accurately discern reasons for a patient's symptoms and history in the event of an acute illness. It is specifically adapted to elicit symptoms of a possible heart attack. Each letter stands for an important line of questioning for the patient assessment. This is usually taken along with vital signs and the SAMPLE history and would usually be recorded by the person delivering the aid, such as in the "Subjective" portion of a SOAP note, for later reference. Onset of the event. What the patient was doing when it started (active, inactive, stressed, etc.), whether the patient believes that activity prompted the pain, and whether the onset was sudden, gradual or part of an ongoing chronic problem. Provocation or palliation. Whether any movement, pressure (such as palpation) or other external factor makes the problem better or worse. This can also include whether the symptoms relieve with rest. Quality of the pain. This is the patient's description of the pain. Questions can be open ended ("Can you describe it for me?") or leading. Ideally, this will elicit descriptions of the patient's pain: whether it is sharp, dull, crushing, burning, tearing, or some other feeling, along with the pattern, such as intermittent, constant, or throbbing. Region and radiation. Where the pain is on the body and whether it radiates (extends) or moves to any other area. This can give indications for conditions such as a myocardial infarction, which can radiate through the jaw and arms. Other referred pains can provide clues to underlying medical causes. Severity. The pain score (usually on a scale of 0 to 10). Zero is no pain and ten is the worst possible pain. This can be comparative (such as "... compared to the worst pain you have ever experienced") or imaginative ("... compared to having your arm ripped off by an alien"). If the pain is compared to a prior event, the nature of that event may be a follow-up question. The clinician must decide whether a score given is realistic within their experience – for instance, a pain score 10 for a stubbed toe is likely to be exaggerated. This may also be assessed for pain now, compared to pain at time of onset, or pain on movement. There are alternative assessment methods for pain, which can be used where a patient is unable to vocalise a score. One such method is the Wong-Baker faces pain scale. Time (history). How long the condition has been going on and how it has changed since onset (better, worse, different symptoms), whether it has ever happened before, whether and how it may have changed since onset, and when the pain stopped if it is no longer currently being felt.
Lab Work - Screening
Laboratory is a facility that provides controlled conditions in which scientific or technological research, experiments, and measurement may be performed. Analytical Chemistry.
Medical Laboratory is a laboratory where tests are usually done on clinical specimens in order to obtain information about the health of a patient as pertaining to the diagnosis, treatment, and prevention of disease. Clinical laboratories are thus focused on applied science mainly on a production-like basis, as opposed to research laboratories that focus on basic science on an academic basis. Forensic Science.
Lab Tests - Blood Test - Urinalysis - Pee - Poop
Lab Tests Online - Direct Labs - Lab Test Portal
Quest Diagnostics - Clinical Trials - Berkeley Laboratory
Nelson Labs - Clinical Laboratory Manage - Lab Calibrations
Screening in medicine is a strategy used in a population to identify the possible presence of an as-yet-undiagnosed disease in individuals without signs or symptoms. This can include individuals with pre-symptomatic or unrecognized symptomatic disease. As such, screening tests are somewhat unusual in that they are performed on persons apparently in good health. Screening interventions are designed to identify disease in a community early, thus enabling earlier intervention and management in the hope to reduce mortality and suffering from a disease. Although screening may lead to an earlier diagnosis, not all screening tests have been shown to benefit the person being screened; Over-Diagnosis, Mis-Diagnosis, and creating a false sense of security are some potential adverse effects of screening. Additionally, some screening tests can be inappropriately overused. For these reasons, a test used in a screening program, especially for a disease with low incidence, must have good sensitivity in addition to acceptable specificity. Several types of screening exist: universal screening involves screening of all individuals in a certain category (for example, all children of a certain age). Case finding involves screening a smaller group of people based on the presence of risk factors (for example, because a family member has been diagnosed with a hereditary disease). Screening interventions are not designed to be diagnostic, and often have significant rates of both false positive and false negative results.
Bioinformatics are methods and software tools for understanding biological data.
Assessment Errors (observation flaws) - Testing Vulnerabilities - Invitro (vitro)
Clinical Laboratory Research is a branch of healthcare science that determines the safety and effectiveness of medications, devices, diagnostic products and treatment regimens intended for human use. These may be used for prevention, treatment, diagnosis or for relieving symptoms of a disease.
Endopat non-invasive assessment of Endothelial Dysfunction (arterial health), is a functional test for early detection of underlying disease progression.
Pathology is a significant component of the causal study of disease and a major field in modern medicine and diagnosis.
Microbiological Culture is a method of multiplying Microbial organisms by letting them reproduce in predetermined culture medium under controlled laboratory conditions. Microbial cultures are foundational and basic diagnostic methods used extensively as a research tool in molecular biology. Microbial cultures are used to determine the type of organism, its abundance in the sample being tested, or both. It is one of the primary diagnostic methods of microbiology and used as a tool to determine the cause of infectious disease by letting the agent multiply in a predetermined medium. For example, a throat culture is taken by scraping the lining of tissue in the back of the throat and blotting the sample into a medium to be able to screen for harmful microorganisms, such as Streptococcus pyogenes, the causative agent of strep throat. Furthermore, the term culture is more generally used informally to refer to "selectively growing" a specific kind of microorganism in the lab. It is often essential to isolate a pure culture of microorganisms. A pure (or axenic) culture is a population of cells or multicellular organisms growing in the absence of other species or types. A pure culture may originate from a single cell or single organism, in which case the cells are genetic clones of one another. For the purpose of gelling the microbial culture, the medium of agarose gel (agar) is used. Agar is a gelatinous substance derived from seaweed. A cheap substitute for agar is guar gum, which can be used for the isolation and maintenance of thermophiles. Symptoms.
Vitals are body functions essential for life. - Food - First Aid
Public Health Laboratory are governmental reference laboratories that protect the public against diseases and other health hazards.
Association of Public Health Laboratories is a membership organization in the United States representing the laboratories that protect the health and safety of the public.
Public Health Laboratories work at the federal, state and local level, public health laboratories monitor and detect health threats ranging from rabies and dengue fever to radiological contaminants, genetic disorders in newborns and terrorist agents. Equipped with sophisticated instrumentation and staffed by highly trained scientists, these unique institutions deliver services that may be unavailable or cost-prohibitive elsewhere.
Emergency Use Authorizations
Laboratory Response Network Partners is a network of laboratories that can respond to biological and chemical threats and other public health emergencies.
Diagnostic Tests - Advanced Sensors
Biomarker is a measurable indicator of the severity or presence of some disease state. More generally a biomarker is anything that can be used as an indicator of a particular disease state or some other physiological state of an organism.
Heart Diagnostics - Crispr (gene therapy)
Breath Gas Analysis is a method for gaining non-invasive information on the clinical state of an individual by monitoring volatile organic compounds present in the exhaled breath. Breath gas concentration can then be related to blood concentrations via mathematical modeling as for example in blood alcohol testing. Breathalyzers.
Breath Test could be possible for Drugs and Disease. The versatile use of exhaled volatile organic compounds in human health and disease. Exhaled breath contains thousands of volatile organic compounds (VOCs) of which the composition varies depending on health status. Various metabolic processes within the body produce volatile products that are released into the blood and will be passed on to the airway once the blood reaches the lungs. Moreover, the occurrence of chronic inflammation and/or oxidative stress can result in the excretion of volatile compounds that generate unique VOC patterns. Consequently, measuring the total amount of VOCs in exhaled air, a kind of metabolomics also referred to as breathomics.
Lab on a Chip is a device that integrates one or several laboratory functions on a single integrated circuit (commonly called a "chip") of only millimeters to a few square centimeters to achieve automation and high-throughput screening. LOCs can handle extremely small fluid volumes down to less than pico liters. Lab-on-a-chip devices are a subset of micro-electro-mechanical systems (MEMS) devices and sometimes called "micro total analysis systems" (µTAS). LOCs may use microfluidics, the physics, manipulation and study of minute amounts of fluids. However, strictly regarded "lab-on-a-chip" indicates generally the scaling of single or multiple lab processes down to chip-format, whereas "µTAS" is dedicated to the integration of the total sequence of lab processes to perform chemical analysis. The term "lab-on-a-chip" was introduced when it turned out that µTAS technologies were applicable for more than only analysis purposes. Sensors (AI).
Jack Andraka (video and text) - Body Parts on a Chip (video and text)
Microfluidics deals with the behaviour, precise control and manipulation of fluids that are geometrically constrained to a small, typically sub-millimeter, scale. Lego.
Organ on a Chip is a multi-channel 3-D microfluidic cell culture chip that simulates the activities, mechanics and physiological response of entire organs and organ systems, a type of artificial organ. Personalized Medicine.
Scientists design built-in controls for mini-chemical labs on a chip. In a miniaturized laboratory, microfluidic systems can conduct chemical experiments on a chip through a series of small connected tubes the size of a hair.
Smartphone Tools - Smartphone Apps
Sensors woven into a shirt can monitor vital signs such as temperature, respiration, and heart rate.
Biosense
Bio-Sensor Patch Monitor
Wearable Sensors
GlucoWatch G2 Biographer
Diagnostic Paper, Whiteside's
Electrochemical Sensing in Paper-Based Microfluidic Device
Claros Diagnostic Lab
Materials that Compute
Paper Test Strip for Diagnosing Diseases
Ph Levels
Variable Tech Gadgets
DxtER
Telemedicine (in-home patient monitoring system)
Addressing Antibiotic Resistance: Breath Analysis aims to reduce unnecessary prescriptions. Scientists have found a potentially useful link between the presence of exhaled acinetobacter baumannii derived volatile organic compounds (VOCs) and patients diagnosed with bacterial pneumonia.
Flexible Electronics - Software Testing
Capturing Brain Signals with Soft Electronics using long-term stable neural recording based on a novel elastic material composite, which is biocompatible and retains high electrical conductivity even when stretched to double its original length.
A self-Healing Sweat Sensor. Wearable sensors that track heart rate or steps are popular fitness products. But in the future, working up a good sweat could provide useful information about a person's health. Now, researchers have developed a headband that measures electrolyte levels in sweat. And unlike many previous sweat sensors, the device can heal itself when cut or scratched during exercise.
Smartwatch tracks medication levels to personalize treatments. Advance could help doctors choose the right drug at the right dose for the right person.
Stretchable Biofuel Cells extract Energy from Sweat to power Wearable Devices. A team of engineers has developed stretchable fuel cells that extract energy from sweat and are capable of powering electronics, such as LEDs and Bluetooth radios. The biofuel cells generate 10 times more power per surface area than any existing wearable biofuel cells. The devices could be used to power a range of wearable devices.
Stretchable micro-supercapacitors to self-power wearable devices. A stretchable system that can harvest energy from human breathing and motion for use in wearable health-monitoring devices may be possible, according to an international team of researchers. By using non-layered, ultrathin zinc-phosphorus nanosheets and 3D laser-induced graphene foam -- a highly porous, self-heating nanomaterial -- to construct the island-bridge design of the cells, Cheng and his team saw drastic improvements in electric conductivity and the number of absorbed charged ions. This proved that these micro-supercapacitor arrays can charge and discharge efficiently and store the energy needed to power a wearable device. The researchers also integrated the system with a triboelectric nanogenerator, an emerging technology that converts mechanical movement to electrical energy. This combination created a self-powered system.
Self-Powered Paper-Based Electrochemical Devices 'SPEDs' may lead to new medical-diagnostic tools. A new medical-diagnostic device made out of paper detects biomarkers and identifies diseases by performing electrochemical analyses -- powered only by the user's touch -- and reads out the color-coded test results, making it easy for non-experts to understand. The top layer of the SPED is fabricated using untreated cellulose paper with patterned hydrophobic "domains" that define channels that wick up blood samples for testing. These "microfluidic channels" allow for accurate assays that change color to indicate specific testing results. A machine-vision diagnostic application also was created to automatically identify and quantify each of these "colorimetric" tests from a digital image of the SPED, perhaps taken with a cellphone, to provide fast diagnostic results to the user and to facilitate remote-expert consultation. The bottom layer of the SPED is a "triboelectric generator," or TEG, which generates the electric current necessary to run the diagnostic test simply by rubbing or pressing it. The researchers also designed an inexpensive handheld device called a potentiostat, which is easily plugged into the SPED to automate the diagnostic tests so that they can be performed by untrained users. The battery powering the potentiostat can be recharged using the TEG built into the SPEDs. The SPEDs were used to detect biomarkers such as glucose, uric acid and L-lactate, ketones, and white blood cells, which indicate factors related to liver and kidney function, malnutrition and anemia. Future versions of the technology will contain several additional layers for more complex assays to detect diseases such as dengue fever, yellow fever, malaria, HIV and hepatitis.
Beautifully Designed, Human-Centered Technologies (Shift Labs)
Food Sensors - Sensors (ai)
Drug-delivery system can help even without drugs. A synthetic, injectable hydrogel developed to deliver drugs and encourage tissue growth turns out to have therapeutic properties all its own. encouraged blood vessel and cell growth as new tissue replaced the degrading gel.
Telemedicine - In-Home Monitoring - Doctor House Calls
Patient Monitoring Remotely can improve patient care and reduce costs. The ability to monitor the patient’s condition remotely not only enhances the quality of care, it also improves clinical efficiency and it can substantially reduce healthcare costs in multiple ways. It reduces the number of in-hospital device evaluations, hospital admissions, the length of stay hospitalization, and follow-up office visits.
Monitoring in medicine is the observation of a disease, condition or one or several medical parameters over time. It can be performed by continuously measuring certain parameters or vital signs using a medical monitor or bedside monitor. This may include repeatedly performing medical tests such as blood glucose monitoring with a glucose meter in people with diabetes mellitus. Transmitting data from a monitor to a distant monitoring station is known as telemetry or biotelemetry.
Remote Patient Monitoring is a technology to enable monitoring of patients outside of conventional clinical settings such as in their home, which may increase access to care and decrease healthcare delivery costs. Incorporating RPM in chronic disease management can significantly improve an individual's quality of life. It allows patients to maintain independence, prevent complications, and minimize personal costs. RPM facilitates these goals by delivering care right to the home. In addition, patients and their family members feel comfort knowing that they are being monitored and will be supported if a problem arises. This is particularly important when patients are managing complex self-care processes such as home hemodialysis. Key features of RPM, like remote monitoring and trend analysis of physiological parameters, enable early detection of deterioration; thereby, reducing number of emergency department visits, hospitalizations, and duration of hospital stays. The need for wireless mobility in healthcare facilitates the adoption of RPM both in community and institutional settings. The time saved as a result of RPM implementation increases efficiency, and allows healthcare providers to allocate more time to remotely educate and communicate with patients. Wearable Sensors (AI).
Visiting Nurses - Home Monitors (caregiving from a distance) - Health Apps - Apps.
House Call is a visit to the home of a patient or client by a Doctor or other professional. In some locations, families used to pay dues to a particular practice to underwrite house calls.
Point of Care is the point in time when clinicians deliver healthcare products and services to patients at the time of care. Point of care documentation is the ability for clinicians to document clinical information while interacting with and delivering care to patients. A clinician will create clinical documentation, which is a record of the critical thinking and judgment of a health care professional, facilitating consistency and effective communication among clinicians and patients. Documentation should be performed at the time of clinical point of care and can be conducted using paper or electronic formats. This process aims to capture medical information pertaining to patient's healthcare needs. The patient's health record is a legal document that contains details regarding patient’s care and progress. The types of information captured during the clinical point of care documentation include the actions taken by clinical staff including physicians and nurses, and the patient’s healthcare needs, goals, diagnosis and the type of care they have received from the healthcare providers. Such documentations provide evidence regarding safe, effective and ethical care and insinuates accountability for healthcare institutions and professionals. Furthermore, accurate documents provide a rigorous foundation for conducting appropriate quality of care analysis that can facilitate better health outcomes for patients. Thus, regardless of the format used to capture the clinical point of care information, these documents are imperative in providing safe healthcare. Also, it is important to note that electronic formats of clinical point of care documentation are not intended to replace existing clinical process but to enhance the current clinical point of care documentation process. One of the major responsibilities for nurses in healthcare settings is to forward information about the patient's needs and treatment to other healthcare professionals.
Home Hospital Reduces Costs, Improves Care. Utilization, and readmissions while increasing physical activity compared with usual hospital care. The home hospital model of care -- in which select patients receive hospital-level care for an acute illness from the comfort of their own home instead of in a traditional hospital -- has become increasingly popular across the United States. Caregiving.
Outpatient is a patient who receives medical treatment without being admitted to a hospital. Outpatients are people with health problems who visit the hospital for diagnosis or treatment, but do not at this time require a bed or need to be admitted for overnight care. Modern outpatient departments offer a wide range of treatment services, diagnostic tests and minor surgical procedures. An out-patient is a patient who attends the hospital with no plan to stay beyond the duration of the visit. Even if the patient will not be formally admitted with a note as an outpatient, their attendance are still registered, and the provider will usually give a note explaining the reason for the visit, tests or procedure/surgery, which should include the names and titles of the participating personnel, the patient's name and date of birth, signature of informed consent, estimated pre- and post-service time for a history and exam (before and after), any anesthesia, medications or future treatment plans needed, and estimated time of discharge absent any (further) complications. Treatment provided in this fashion is called ambulatory care. Sometimes surgery is performed without the need for a formal hospital admission or an overnight stay, and this is called outpatient surgery or "day surgery", which has many benefits including lowered healthcare cost, reducing the amount of medication prescribed and using the physician's or surgeon's time more efficiently. Outpatient surgery is suited best for more healthy patients undergoing minor or intermediate procedures (limited urologic, ophthalmologic, or ear, nose and throat procedures and procedures involving superficial skin and the extremities). More procedures are being performed in a surgeon's office, termed office-based surgery, rather than in a hospital-based operating room.
Ambulatory Care is medical care provided on an outpatient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services. This care can include advanced medical technology and procedures even when provided outside of hospitals. Many medical investigations and treatments for acute and chronic illnesses and preventive health care can be performed on an ambulatory basis, including minor surgical and medical procedures, most types of dental services, dermatology services, and many types of diagnostic procedures (e.g. blood tests, X-rays, endoscopy and biopsy procedures of superficial organs). Other types of ambulatory care services include emergency visits, rehabilitation visits, and in some cases telephone consultations. Ambulatory care services represent the most significant contributor to increasing hospital expenditures and to the performance of the health care system in most countries, including most developing countries.
Street Medicine Institute Street medicine practice is defined as those health care and related services that are delivered directly to persons sleeping on the streets, along the river banks, and in the abandoned buildings, etc., of cities. Street Medicine.
E-Patient is a health consumer who participates fully in his/her medical care, primarily by gathering information about medical conditions that impact them and their families, using the Internet and other digital tools. Good Doctors Ratings.
M-Health is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and PDAs, and wearable devices such as smart watches, for health services, information, and data collection. The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information. mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery of healthcare information to practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care (via mobile telemedicine) as well as training and collaboration of health workers.
E-Health is a relatively recent healthcare practice supported by electronic processes and communication, dating back to at least 1999.
Therapy delivered electronically more effective than face to face.
Clinical Decision Support System is a means of requesting diagnostic tests and treatments electronically and receiving the results. A health information technology system that is designed to provide physicians and other health professionals with clinical decision support (CDS), that is, assistance with clinical decision-making tasks.
Computerized Physician Order Entry is a means of requesting diagnostic tests and treatments electronically and receiving the results.
Telemedicine is the use of smartphone telecommunication and computers with internet to provide clinical health care from a distance. It has been used to overcome distance barriers and to improve access to medical services that would often not be consistently available in distant rural communities. It is also used to save lives in critical care and emergency situations. Telemedicine is remote clinical services, such as diagnosis and monitoring, while telehealth includes preventative, promotive, and curative care delivery. The World Health Organization uses telemedicine to describe all aspects of health care including preventive care. Telehealth can include non-clinical services, such as provider training, administrative meetings, and continuing medical education, and that the term telemedicine means remote clinical services. Telehealth requires a strong, reliable broadband connection. As broadband infrastructure has improved, telehealth usage has become more widely feasible. Store and forward telemedicine involves acquiring medical data (like medical images, biosignals etc.) and then transmitting this data to a doctor or medical specialist at a convenient time for assessment offline. It does not require the presence of both parties at the same time. Remote monitoring, also known as self-monitoring or testing, enables medical professionals to monitor a patient remotely using various technological devices. Telenutrition refers to the use of video conferencing/ telephony to provide online consultation by a nutritionist or dietician. Telenursing refers to the use of telecommunications and information technology in order to provide nursing services in health care whenever a large physical distance exists between patient and nurse, or between any number of nurses. Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist.
Telemedicine - The Disappearance of the Primary Care Physical Examination—Losing Touch.
Video Chat with a Doctor - Tele-Medicine Exchange - Capture Proof
Teladoc 24/7 Access to a Doctor via Phone and Online Video Consultations.
Virtual Doctor MD - Physicians Online - Interactive MD - Online Care over the Internet
Biotelemetry involves the application of telemetry in biology, medicine, and other health care to remotely monitor various vital signs of ambulatory patients. A typical biotelemetry system comprises: Sensors appropriate for the particular signals to be monitored. Battery-powered, Patient worn transmitters. A Radio Antenna and Receiver. A display unit capable of concurrently presenting information from multiple patients.
Electronic Prescribing is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions.
Health Informatics is information engineering applied to the field of health care, essentially the management and use of patient healthcare information.
Consumer Health Informatics use of electronic resources on medical topics by healthy individuals or patients.
Boston Scientific Latitude NXT in-home patient monitoring system allows a healthcare team to monitor connected devices in-between primary care visits. Devices send data to providers at regularly scheduled times from blood pressure monitors, pacemakers, cardiac monitors, weight scales, and other connected health devices. The NXT connector is hands-free, meaning that patients do not have to intervene to send health data. Vital Signs - Sleep Monitors.
Doctor on Demand US-based, board-certified Doctors and Licensed Psychologists are available on your Schedule.
Doctors without Borders
Medical Aid App (youtube)
Health Symptoms Checker - Risk Assessment
Health Loop in patient engagement solutions for providers, patients and their families. Cloud-based platform that automates follow-up care.
GE Healthcare Apex Pro CH telemetry system that allows hospitals and other healthcare organizations to unify their monitoring systems under a single wireless network.
Medtronic Vital Sync monitoring platform providers integrated physiological information from bedside monitors and wearable devices to a hospital server.
Nihon Koden Aware alarm management system allows hospitals to draw analytics from their monitoring parameters, and see detailed information about the types of patients and when patients experience health risks. Aware is intended to assist providers in identifying which alarms need the most attention based upon patient condition. Providers can also use the system to detect when alarms are on, off, have low battery life, and telemetry alarm responses.
EncorePro 2 has all a patient’s data presented in one convenient dashboard while automating routine sleep and respiratory settings.
Remote Monitoring - Telemetry - Tele-Robotics
Text messaging intervention is the next generation of therapy in mental health. A psychotherapy tool in real-time. Text-messaging as an add-on to an assertive community treatment. Today, there are more than 575,000 mental health therapists in the U.S. By 2025, the U.S. Department of Health and Human Services estimates that the country will be over 250,000 therapists short. "A messaging-based intervention is an incredibly scalable, cost-effective way to help manage the enormous shortage of mental health capability in the U.S.
Surgery
 Surgery is a
medical specialty that uses operative
manual and instrumental techniques on a person to investigate or treat
a pathological condition such as a disease or injury, to help improve
bodily function or appearance or to repair unwanted ruptured areas. The
act of performing surgery may be called a surgical
procedure, operation, or simply
"surgery". In this context, the verb "operate"
means to perform surgery. The adjective surgical means pertaining to
surgery; e.g.
surgical instruments or
surgical nurse. The person or subject on which the surgery is
performed can be a person or an animal. A surgeon is a person who
practices surgery and a surgeon's assistant is a person who practices
surgical assistance. A surgical team is made up of surgeon, surgeon's
assistant, anaesthetist, circulating nurse and
surgical technologist. Surgery usually spans minutes to hours, but it is
typically not an ongoing or periodic type of treatment. The term "surgery"
can also refer to the place where surgery is performed, or, in British
English, simply the office of a physician, dentist, or veterinarian.
Surgery is a
medical specialty that uses operative
manual and instrumental techniques on a person to investigate or treat
a pathological condition such as a disease or injury, to help improve
bodily function or appearance or to repair unwanted ruptured areas. The
act of performing surgery may be called a surgical
procedure, operation, or simply
"surgery". In this context, the verb "operate"
means to perform surgery. The adjective surgical means pertaining to
surgery; e.g.
surgical instruments or
surgical nurse. The person or subject on which the surgery is
performed can be a person or an animal. A surgeon is a person who
practices surgery and a surgeon's assistant is a person who practices
surgical assistance. A surgical team is made up of surgeon, surgeon's
assistant, anaesthetist, circulating nurse and
surgical technologist. Surgery usually spans minutes to hours, but it is
typically not an ongoing or periodic type of treatment. The term "surgery"
can also refer to the place where surgery is performed, or, in British
English, simply the office of a physician, dentist, or veterinarian. Surgeon is a doctor who performs operations, which is a medical procedure involving an incision using instruments in order to repair damage or arrest disease in a living body. Incision is cutting into body tissues or organs. Surgeons may be physicians, podiatrists, dentists, or veterinarians. Robotic Surgery.
Invasive Surgical Procedure refers to surgical techniques that limit the size of incisions needed and so lessens wound healing time, associated pain and risk of infection. An endovascular aneurysm repair as an example of minimally invasive surgery is much less invasive in that it involves much smaller incisions, than the corresponding open surgery procedure of open aortic surgery.
 Surgery Encyclopedia
Surgery EncyclopediaUniversal Anesthesia Machine
Onebreath low-cost Ventilator
Surgery Simulator
Color Coded Surgery (video)
Ultrasound Surgery (video) - Web
O-Arm Surgical Imaging
Laparoscopic
3D Holographic Imaging
Body Browser (youtube)
Surgery Costs by State - Health Cost Institute - Fraud
Female surgeons earned 24% less per hour while operating compared to male surgeons.
Molecular Surgery reshapes living tissue with electricity but No Incisions. Researchers have developed a 'molecular surgery' process using tiny needles, electric current and 3D molds to quickly reshape living tissue with no incisions, scarring or recovery time. It shows promise as a noninvasive alternative to laser eye surgery.
Implant Infections could be banished thanks to Scaffold Breakthrough. A new type of implant scaffold to provide localised drug treatment and prevent infection. Battling bacterial infection with hexamethylene diisocyanate cross-linked and Cefaclor-loaded collagen scaffolds.
Replantation the surgical reattachment of a body part, most commonly a finger, hand or arm, that has been completely cut from a person's body. Replantation of amputated parts has been performed on fingers, hands, forearms, arms, toes, feet, legs, ears, avulsed scalp injuries, a face, lips, penis and a tongue. It can be performed on almost any body part of children. Regeneration.
Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene.
Surgical Stress is the systemic response to surgical injury and is characterized by activation of the sympathetic nervous system, endocrine responses as well as immunological and haematological changes. Measurement of surgical stress is used in anaesthesia, physiology and surgery. Analysis of the surgical stress response can be used for evaluation of surgical techniques and comparisons of different anaesthetic protocols. Moreover, they can be performed both in the intraoperative or postoperative period. If there is a choice between different techniques for a surgical procedure, one method to evaluate and compare the surgical techniques is to subject one group of patients to one technique, and the other group of patients to another technique, after which the surgical stress responses triggered by the procedures are compared. The technique with the least surgical stress response is considered the best for the patient. Similarly, a group of patients can be subjected to a surgical procedure where one anaesthetic protocol is used, and another group of patients are subjected to the same surgical procedure but with a different anaesthetic protocol. The anaesthetic protocol that yields the least stress response is considered the most suitable for that surgical procedure. It is generally considered or hypothesized that a more invasive surgery, with extensive tissue trauma and noxious stimuli, triggers a more significant stress response. However, duration of surgery may affect the stress response which therefore may make comparisons of procedures that differ in time difficult.
Medical Procedure is a course of action intended to achieve a result in the delivery of healthcare. A medical procedure with the intention of determining, measuring, or diagnosing a patient condition or parameter is also called a medical test. Other common kinds of procedures are therapeutic (i.e., intended to treat, cure, or restore function or structure), such as surgical and physical rehabilitation procedures.
Organ Transplants
Organ Transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location. Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source. T-Cells.
Organ Donation is when a person allows to be removed, legally, either by consent while the donor is alive or after death with the assent of the next of kin. Donation may be for research, or, more commonly healthy transplantable organs and tissues may be donated to be transplanted into another person. Common transplantations include: kidneys, heart, liver, pancreas, intestines, lungs, bones, bone marrow, skin, and corneas. Some organs and tissues can be donated by living donors, such as a kidney or part of the liver, but most donations occur after the donor has died. As of August 1, 2016, there are 120,004 people waiting for life-saving organ transplants in the US. Of these, 96,645 await kidney transplants. While views of organ donation are positive there is a large gap between the numbers of registered donors compared to those awaiting organ donations on a global level.
Presumed consent is alternatively known as an 'opt-out' system and means that unless the deceased has expressed a wish in life not to be an organ donor then consent will be assumed. In opt-out systems, organ donation will occur automatically unless a specific request is made before death for organs not to be taken.
120,000 Americans are on organ transplant waiting lists. 20 people die every day from the lack of available organs for transplant. 30 Americans a day either die on the waiting list or are removed from it because they have become too ill to receive a transplant. Every day, over 75 people in the United States get an organ transplant. About 130 new people are put on transplant waiting lists each day.
One Legacy - Organ Donor (gov)
Paired Donation - Paired Kidney Exchange
Scientists Triple Storage Time of Human Donor Livers. Research project develops new method to preserve human livers for transplantation. A new method of preservation maintains human liver tissue for up to 27 hours will give doctors and patients a much longer timeframe for organ transplant. They were able to do this by adding a modified glucose compound, 3-OMG, and PEG-35kD -- an ingredient in antifreeze -- to the protective solution that they use to cool the livers. The PEG compound lowers the temperature at which the cells freeze and 3-OMG acts as a protectant against the cold. With these additions, they were able to cool the rat livers to ?6 degrees Celsius without freezing them -- a process called supercooling.
Matching Donors and Recipients, These usually include: Blood type, Body size, Severity of patient's medical condition, Distance between the donor's hospital and the patient's hospital, The patient's waiting time, Whether the patient is available (for example, whether the patient can be contacted and has no current infection or other temporary reason that transplant cannot take place). Depending on the organ, however, some factors become more important. For example, some organs can survive outside the body longer than others. So the distance between the donor's hospital and the potential recipient's hospital must be taken into consideration.
Can an organ recipient choose an organ from a younger person? Putting a kidney from a 70 year old donor into a 20 year old recipient is not a great idea. In the reverse situation a 20 year old kidney transplanted into a 70 year old will be exposed to an aging environment: high blood pressure, other organs which are not functioning optimally and it will not last as long as it would in a 20 year old recipient (assuming the etiology is not prone to recurrence). A 70 year old kidney would probably last longer in a 20 year old than in another 70 year old but sometimes young and otherwise healthy patients have a greater tendency to reject than older ones. In any case, some sort of age matching makes sense if feasible. The biological age of the transplanted organ won't change after it has been transplanted. Almost everyone can be an organ donor, no matter what your age.
Can people of different races and ethnicities match each other? Yes. People of different ethnicities frequently match each other. How are donated organs distributed? Organs are matched to patients based on a number of factors, including blood and tissue typing, medical need, time on the waiting list, and geographical location.
More than 100,000 people in the United States are waiting for a new kidney. 500,000 are on dialysis.
Living Donations of a kidney can be made to a family member, friend, or anyone on the waiting list.
Dialysis is a process for removing waste and excess water from the blood and is used primarily as an artificial replacement for lost kidney function in people with kidney failure. Dialysis may be used for those with an acute disturbance in kidney function (acute kidney injury, previously acute renal failure) or progressive but chronically worsening kidney function—a state known as chronic kidney disease stage 5 (previously chronic kidney failure or end-stage renal disease).
Dialysis: Last Week Tonight with John Oliver (HBO) (youtube)
Allotransplantation is the transplantation of cells, tissues, or organs, to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, or homograft. Most human tissue and organ transplants are allografts.
Xenotransplantation is the transplantation of living cells, tissues or organs from one species to another. Such cells, tissues or organs are called xenografts or xenotransplants. It is contrasted with allotransplantation (from other individual of same species), Syngeneic transplantation (Grafts transplanted between two genetically identical individuals of the same species) and Autotransplantation (from one part of the body to another in the same person).
Porcine Endogenous Retroviruses are remnants of ancient viral infections, found in the genomes of most, if not all, mammalian species. Integrated into the chromosomal DNA, they are vertically transferred through inheritance.[26] Due to the many deletions and mutations they accumulate over time, they usually are not infectious in the host species, however the virus may become infectious in another species.
Transplant Recipients Receive Memories of the Organ Donor
Circumventricular Organs are structures in the brain that are characterized by their extensive vasculature and lack of a normal blood brain barrier (BBB). The CVOs allow for the linkage between the central nervous system and peripheral blood flow; additionally they are an integral part of neuroendocrine function. The lack of a blood brain barrier allows the CVOs to act as an alternative route for peptides and hormones in the neural tissue to the peripheral blood stream, while still protecting it from toxic substances. CVOs can be classified as either sensory or secretory organs. The sensory organs include the area postrema (AP), the subfornical organ (SFO) and the vascular organ of lamina terminalis. They have the ability to sense plasma molecules and then pass that information into other regions of the brain. Through this, they provide direct information to the autonomic nervous system from the systemic circulation. The secretory organs include the subcommissural organ (SCO), the posterior pituitary, the pineal gland, the median eminence and the intermediate lobe of the pituitary gland. These organs are responsible for secreting hormones and glycoproteins into the peripheral vascular system using feedback from both the brain environment and external stimuli. All of the circumventricular organs, besides the SCO, contain extensive vasculature and fenestrated capillaries which leads to a ‘leaky’ BBB at the site of the organs. Furthermore, all CVOs contain neural tissue, allowing them to play a role in the neuroendocrine system. It is highly debated if the choroid plexus can be included as a CVO. It has a high concentration of fenestrated capillaries, but its lack of neural tissue and its primary role of producing cerebrospinal fluid (CSF) usually excludes the choroid plexus from the CVO classification. Research has also linked CVOs to body fluid regulation, cardiovascular functions, immune responses, thirst, feeding behavior and reproductive behavior.
Secretory Organ is any of various organs that synthesize substances needed by the body and release it through ducts or gland or directly into the bloodstream.
Situs Inversus is a congenital condition in which the major visceral organs are reversed or mirrored from their normal positions. The normal arrangement of internal organs is known as situs solitus while situs inversus is generally the mirror image of situs solitus. Although cardiac problems are more common than in the general population, most people with situs inversus have no medical symptoms or complications resulting from the condition, and until the advent of modern medicine it was usually undiagnosed.
Microparticles show promise for Transplant Rejection
Lifesaving Organs for Transplant sometimes go Missing in Transit. Hearts survive only four to six hours out of the body. And kidneys and pancreases have longer shelf lives and often travel commercial, as cargo. As such, they can end up missing connecting flights or delayed like lost luggage. Worse still, they are typically tracked with a primitive system of phone calls and paper manifests, with no GPS or other electronic tracking required. We’ve had organs that are left on airplanes, organs that arrive at an airport and then can’t get taken off the aircraft in a timely fashion and spend an extra two or three or four hours waiting for somebody to get them. Organ Procurement Organizations often rely on commercial couriers and airlines, which are not formally held accountable for any ensuing problems. If an airline forgets to put a kidney on a plane or a courier misses a flight because he got lost or stuck in traffic, there is no consequence. If Amazon can figure out when your paper towels and your dog food is going to arrive within 20 to 30 minutes, it certainly should be reasonable that we ought to track lifesaving organs, which are in chronic shortage.
Harvested alive -10 years investigation of Force Organ Harvesting (youtube) - China has been harvesting organs from live prisoners to create it's thriving transplant industry. Average wait time for a liver in the US is 24-36 MONTHS. Average wait time in China is 14-21 DAYS. HARD TO BELIEVE - Chapter 3 - The Canadian Investigation (youtube).
Organ Transplantation in China has taken place since the 1960s, and is one of the largest organ transplant programmes in the world, peaking at over 13,000 liver and kidney transplants a year in 2004. China is also involved in innovative transplant surgery such as face transplantation including bone.
Organ Procurement or Organ Harvesting is a surgical procedure that removes organs or tissues for reuse, typically for organ transplantation. If the organ donor is human, most countries require that the donor be legally dead for consideration of organ transplantation (e.g. cardiac or brain dead). For some organs, a living donor can be the source of the organ. For example, living donors can donate one kidney or part of their liver to a well-matched recipient.
Transplant Tourism in the United States: A Single-Center Experience. The practice of traveling outside the country of residence to obtain organ transplantation.
Food - Nutrition
Exercise - Sports
Human Body Knowledge
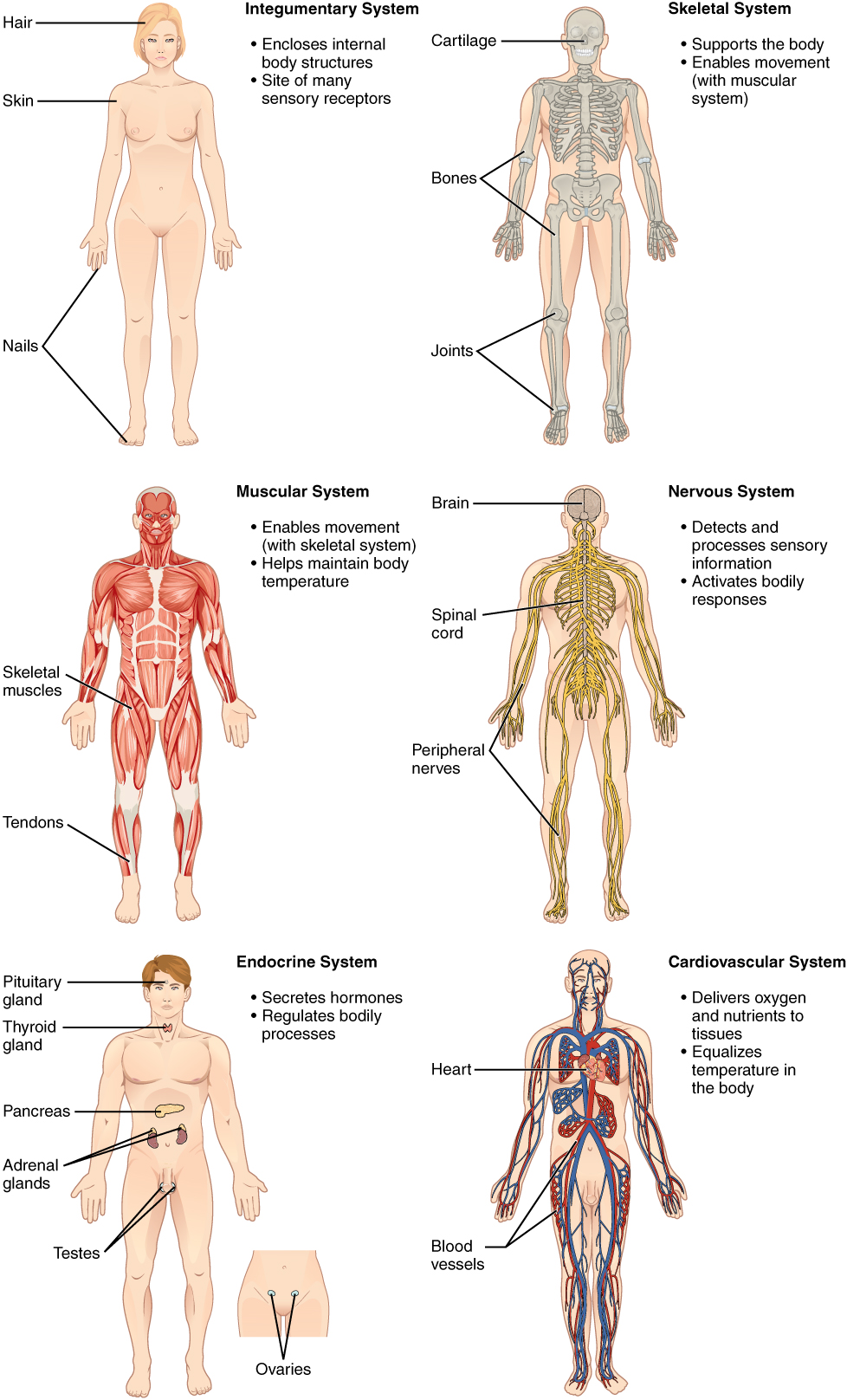 Human Body is the entire structure
of a human being. It is composed of many different types of
cells that
together create tissues and subsequently organ
systems. They ensure
homeostasis and viability of human body. It comprises a
head, neck, trunk, which includes the
thorax and
abdomen, arms and
hands, legs and
feet, and skin.
The study of the human body involves anatomy, physiology, histology and
embryology. The body varies anatomically in known ways.
Human Body is the entire structure
of a human being. It is composed of many different types of
cells that
together create tissues and subsequently organ
systems. They ensure
homeostasis and viability of human body. It comprises a
head, neck, trunk, which includes the
thorax and
abdomen, arms and
hands, legs and
feet, and skin.
The study of the human body involves anatomy, physiology, histology and
embryology. The body varies anatomically in known ways. Biological Organization is the hierarchy of complex biological structures and systems that define life using a reductionistic approach. The traditional hierarchy extends from atoms to biospheres. The higher levels of this scheme are often referred to as an ecological organization concept, or as the field, hierarchical ecology. Each level in the hierarchy represents an increase in organizational complexity, with each "object" being primarily composed of the previous level's basic unit. The basic principle behind the organization is the concept of emergence—the properties and functions found at a hierarchical level are not present and irrelevant at the lower levels. The biological organization of life is a fundamental premise for numerous areas of scientific research, particularly in the medical sciences. Without this necessary degree of organization, it would be much more difficult—and likely impossible—to apply the study of the effects of various physical and chemical phenomena to diseases and physiology (body function). For example, fields such as cognitive and behavioral neuroscience could not exist if the brain was not composed of specific types of cells, and the basic concepts of pharmacology could not exist if it was not known that a change at the cellular level can affect an entire organism. These applications extend into the ecological levels as well. For example, DDT's direct insecticidal effect occurs at the subcellular level, but affects higher levels up to and including multiple ecosystems. Theoretically, a change in one atom could change the entire biosphere. (Cells - Tissues - Organs - Organ Systems - Organism) - Anatomy is Form and Physiology is Function. Form Influences Function.
Physiology focuses on the systems and organs of the human body and their functions. Many systems and mechanisms interact in order to maintain homeostasis, with safe levels of substances such as sugar and oxygen in the blood. The body is studied by health professionals, physiologists, anatomists, and by artists to assist them in their work. Body Motion. Organ Donation.
Anatomy is the branch of biology concerned with the study of the structure of organisms and their parts. Anatomy is inherently tied to embryology, comparative anatomy, evolutionary biology, and phylogeny, as these are the processes by which anatomy is generated over immediate (embryology) and long (evolution) timescales. Human anatomy is one of the basic essential sciences of medicine. The discipline of anatomy is divided into macroscopic and microscopic anatomy. Macroscopic anatomy, or gross anatomy, is the examination of an animal's body parts using unaided eyesight. Gross anatomy also includes the branch of superficial anatomy. Microscopic anatomy involves the use of optical instruments in the study of the tissues of various structures, known as histology, and also in the study of cells. The history of anatomy is characterized by a progressive understanding of the functions of the organs and structures of the human body. Methods have also improved dramatically, advancing from the examination of animals by dissection of carcasses and cadavers (corpses) to 20th century medical imaging techniques including X-ray, ultrasound, and magnetic resonance imaging. Anatomy and physiology, which study (respectively) the structure and function of organisms and their parts, make a natural pair of related disciplines, and they are often studied together.
Anatomical Terms of Location. All vertebrates including humans have the same basic body plan: they are strictly bilaterally symmetrical in early embryonic stages and largely bilaterally symmetrical in adulthood. If they are divided down the middle, in other words, they have mirror-image left and right halves.
Coronal Plane is any vertical plane that divides the body into ventral and dorsal (belly and back) sections. It is one of the three main planes of the body used to describe the location of body parts in relation to each other.
Sagittal Plane is an anatomical plane which divides the body into right and left parts. The plane may be in the center of the body and split it into two halves (mid-sagittal) or away from the midline and split it into unequal parts (para-sagittal).The anatomical term sagittal was coined by Gerard of Cremona.
Systems of the Human Body
The human body is the ultimate multitasker that coordinates hundreds of important body functions simultaneously every second, like pumping blood through the body, regulating temperature, breathing, sensing, growing hair and shedding skin cells, producing saliva and tears, repairing bones and creating new cells, removing waste and fighting disease, just to name a few.
Cardiovascular - Circulatory System: Circulates blood around the body via the Heart, arteries and veins, delivering oxygen and nutrients to organs and cells and carrying their waste products away.
Blood Vessel are the part of the circulatory system that transports blood throughout the human body. There are three major types of blood vessels: the Arteries, which carry the blood away from the heart; the Capillaries, which enable the actual exchange of water and chemicals between the blood and the tissues; and the veins, which carry blood from the capillaries back toward the heart.
Vasodilation refers to the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins (called venodilators), large arteries, and smaller arterioles. The process is the opposite of vasoconstriction,, which is the narrowing of blood vessels.
Extracellular Fluid denotes all body fluid outside the cells. Total body water in humans makes up between 45 to 75% of total body weight. About two thirds of this is intracellular fluid within cells, and one third is the extracellular fluid. The main component of the extracellular fluid is the interstitial fluid that bathes cells.
Digestive System - Excretory System: Mechanical and chemical processes that provide nutrients via the mouth, esophagus, stomach and intestines. Eliminates waste from the body.
Microbes
Endocrine System: Provides chemical communications within the body using hormones.
Integumentary System - Exocrine System: Skin, hair, nails, sweat and other exocrine glands.
Lymphatic System - Immune System: The system comprising a network of lymphatic vessels that carry a clear fluid called lymph. Defends the body against disease-causing agents. Lymphatic System is part of the circulatory system and a vital part of the immune system, comprising a network of lymphatic vessels that carry a clear fluid called lymph directionally towards the Heart. Unlike the cardiovascular system, the lymphatic system is not a closed system. The human circulatory system processes an average of 20 liters of blood per day through capillary filtration, which removes plasma while leaving the blood cells. Roughly 17 litres of the filtered plasma are reabsorbed directly into the blood vessels, while the remaining three litres remain in the interstitial fluid. One of the main functions of the lymph system is to provide an accessory return route to the blood for the surplus three litres. The other main function is that of defense in the immune system. Lymph is very similar to blood plasma: it contains lymphocytes and other white blood cells. It also contains waste products and cellular debris together with bacteria and proteins. Associated organs composed of lymphoid tissue are the sites of lymphocyte production. Lymphocytes are concentrated in the lymph nodes. The spleen and the thymus are also lymphoid organs of the immune system. The tonsils are lymphoid organs that are also associated with the digestive system. Lymphoid tissues contain lymphocytes, and also contain other types of cells for support. The system also includes all the structures dedicated to the circulation and production of lymphocytes (the primary cellular component of lymph), which also includes the bone marrow, and the lymphoid tissue associated with the digestive system. Blood Brain Barrier. Lymphatic Vessel are thin-walled, valved structures that carry lymph. As part of the lymphatic system, lymph vessels are complementary to the cardiovascular system. Lymph vessels are lined by endothelial cells, and have a thin layer of smooth muscles, and adventitia that bind the lymph vessels to the surrounding tissue. Lymph vessels are devoted to the propulsion of the lymph from the lymph capillaries, which are mainly concerned with absorption of interstitial fluid from the tissues. Lymph capillaries are slightly larger than their counterpart capillaries of the vascular system. Lymph vessels that carry lymph to a lymph node are called the afferent lymph vessel, and one that carries it from a lymph node is called the efferent lymph vessel, from where the lymph may travel to another lymph node, may be returned to a vein, or may travel to a larger lymph duct. Lymph ducts drain the lymph into one of the subclavian veins and thus return it to general circulation. Generally, lymph flows away from the tissues to lymph nodes and eventually to either the right lymphatic duct or the largest lymph vessel in the body, the thoracic duct. These vessels drain into the right and left subclavian veins respectively. Lymph derived from the interstitial fluid, its composition continually changes as the blood and the surrounding cells continually exchange substances with the interstitial fluid. Lymph is collected through lymph capillaries. It is then transported through larger lymphatic vessels to lymph nodes, where it is cleaned by lymphocytes, before emptying ultimately into the right or the left subclavian vein, where it mixes back with the blood.
Muscular System - Skeletal System: Enables the Body to move using Muscles. Bones support the body and its organs.
Bones - Bone Fracture (first aid) - Posture
Skeleton is the body part that forms the supporting structure of an organism. Vertebrate (wiki).
Human Height is the distance from the bottom of the feet to the top of the head in a human body, standing erect. It is measured using a stadiometer, usually in centimetres when using the metric system, or feet and inches when using the imperial system.
Nervous System: Collects and processes information from the senses via nerves and the brain and tells the muscles to contract to cause physical actions.
Renal System - Urinary System: The system where the kidneys filter blood.
Reproductive System: The sex organs required for the production of offspring.
Respiratory System: The lungs and the trachea that bring air into the body. Breathing.
Sensory System: Consists of sensory receptors, neural pathways, and parts of the brain involved in sensory perception.
Nicer Drums (memory technique acronym for ten organ systems). Systems of the Human Body - List (wiki)
1: Cardiovascular / Circulatory system: Circulates blood around the body via the heart, arteries and veins, delivering oxygen and nutrients to organs and cells and carrying their waste products away.
2: Digestive system / Excretory system: Mechanical and chemical processes that provide nutrients via the mouth, esophagus, stomach and intestines. Eliminates waste from the body.
3: Endocrine system: Provides chemical communications within the body using hormones.
4: Integumentary system/ Exocrine system: Skin, hair, nails, sweat and other exocrine glands. Skin
5: Lymphatic system / Immune system: The system comprising a network of lymphatic vessels that carry a clear fluid called lymph. Defends the body against disease-causing agents.
6: Muscular system/Skeletal system: Enables the body to move using muscles. Bones supporting the body and its organs.
7: Nervous system: Collects and processes information from the senses via nerves and the brain and tells the muscles to contract to cause physical actions.
8: Renal system / Urinary system: The system where the kidneys filter blood.
9: Reproductive system: The sex organs required for the production of offspring.
10: Respiratory system: The lungs and the trachea that bring air into the body.
Eyes: Seeing and Sight - Check your Vision
Organs Human Body (wiki) - (there are approximately 79 organs).
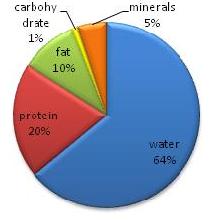 Composition of the Body may be analyzed in terms of
molecular type e.g., water,
protein, connective tissue,
fats (or lipids), hydroxylapatite (in bones),
carbohydrates (such as glycogen and glucose)
and DNA. In terms of tissue type, the body may be analyzed into water,
fat, muscle, bone, etc. In terms of
cell type, the body contains hundreds
of different types of cells, but notably, the largest number of cells
contained in a human body (though not the largest mass of cells)
are not
human cells, but bacteria residing in the normal
human gastrointestinal tract.
Almost 99% of the mass of the human body is made up of six elements:
oxygen, carbon, hydrogen, nitrogen, calcium, and phosphorus. Only about
0.85% is composed of another five elements: potassium, sulfur, sodium,
chlorine, and magnesium. All 11 are necessary for life. The remaining
elements are trace elements, of which more than a dozen are thought on the
basis of good evidence to be necessary for life. All of the mass of the
trace elements put together (less than 10 grams for a human body) do not
add up to the body mass of magnesium, the least common of the 11 non-trace
elements. The average 70 kg (150 lb) adult human body contains
approximately 7×1027 atoms and contains at least detectable traces of 60
chemical elements. About 29 of these elements are thought to play an
active positive role in life and health in humans. The adult human body
averages ~53% water. This varies substantially by age, sex, and adiposity.
In a large sample of adults of all ages and both sexes, the figure for
water fraction by weight was found to be 48 ±6% for females and 58 ±8%
water for males. Water is ~11% hydrogen by mass but ~67% hydrogen by
atomic percent, and these numbers along with the complementary % numbers
for oxygen in water, are the largest contributors to overall mass and
atomic composition figures. Because of water content, the human body
contains more oxygen by mass than any other element, but more hydrogen by
atom-fraction than any element. Some 60 chemical
elements are found in the body, and what all of them are doing
there is mostly unknown.
Composition of the Body may be analyzed in terms of
molecular type e.g., water,
protein, connective tissue,
fats (or lipids), hydroxylapatite (in bones),
carbohydrates (such as glycogen and glucose)
and DNA. In terms of tissue type, the body may be analyzed into water,
fat, muscle, bone, etc. In terms of
cell type, the body contains hundreds
of different types of cells, but notably, the largest number of cells
contained in a human body (though not the largest mass of cells)
are not
human cells, but bacteria residing in the normal
human gastrointestinal tract.
Almost 99% of the mass of the human body is made up of six elements:
oxygen, carbon, hydrogen, nitrogen, calcium, and phosphorus. Only about
0.85% is composed of another five elements: potassium, sulfur, sodium,
chlorine, and magnesium. All 11 are necessary for life. The remaining
elements are trace elements, of which more than a dozen are thought on the
basis of good evidence to be necessary for life. All of the mass of the
trace elements put together (less than 10 grams for a human body) do not
add up to the body mass of magnesium, the least common of the 11 non-trace
elements. The average 70 kg (150 lb) adult human body contains
approximately 7×1027 atoms and contains at least detectable traces of 60
chemical elements. About 29 of these elements are thought to play an
active positive role in life and health in humans. The adult human body
averages ~53% water. This varies substantially by age, sex, and adiposity.
In a large sample of adults of all ages and both sexes, the figure for
water fraction by weight was found to be 48 ±6% for females and 58 ±8%
water for males. Water is ~11% hydrogen by mass but ~67% hydrogen by
atomic percent, and these numbers along with the complementary % numbers
for oxygen in water, are the largest contributors to overall mass and
atomic composition figures. Because of water content, the human body
contains more oxygen by mass than any other element, but more hydrogen by
atom-fraction than any element. Some 60 chemical
elements are found in the body, and what all of them are doing
there is mostly unknown.Chemical Elements listed by their presence in human body - Photo
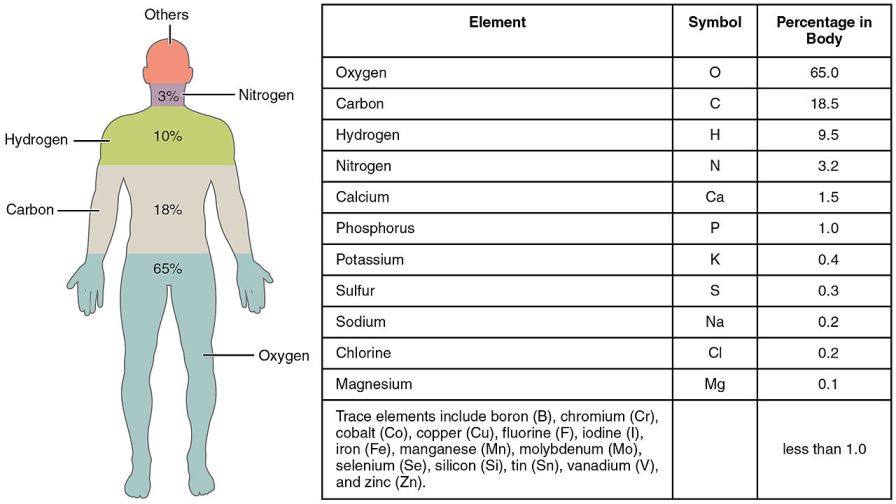 Almost 99% of the mass of the human body is made up of six elements:
oxygen, carbon,
hydrogen,
nitrogen,
calcium, and
phosphorus. Only about
0.85% is composed of another five elements: potassium, sulfur, sodium,
chlorine, and magnesium. A 70 kg (154 lb body) would have approximately 7*1027
atoms. That is, 7 followed by 27 zeros.
Almost 99% of the mass of the human body is made up of six elements:
oxygen, carbon,
hydrogen,
nitrogen,
calcium, and
phosphorus. Only about
0.85% is composed of another five elements: potassium, sulfur, sodium,
chlorine, and magnesium. A 70 kg (154 lb body) would have approximately 7*1027
atoms. That is, 7 followed by 27 zeros.Protons Neutrons Electrons
Hydrogen 4.7*1027 0 4.7*1027
Oxygen 1.4*1028 1.4*1028 1.4*1028
Carbon 4.2*1027 4.2*1027 4.2*1027
Total 2.3*1028 1.8*1028 2.3*1028
98% of the Atoms in your Body will Cycle Out within 1 Year. Full body mass is replaced in 2 weeks. Almost every Cell in the Human Body gets Replaced Every 7 to 10 Years - Body Rejuvenation (video).
Human Bio-Digital
Human Sexuality - Female - Male
Human Body for Kids - Body Browser (youtube)
Human Images From World’s 1st Total-Body Scanner Unveiled. EXPLORER is a combined positron emission tomography (PET) and X-ray computed tomography (CT) scanner that can image the entire body at the same time. Because the machine captures radiation far more efficiently than other scanners, EXPLORER can produce an image in as little as 1 second and, over time, produce movies that can track specially tagged drugs as they move around the entire body.
Skin Color
Human Skin Color ranges in variety from the darkest brown to the lightest hues. An individual's skin pigmentation is the result of genetics, being the product of both of the individual's biological parents' genetic makeup. In evolution, skin pigmentation in human beings evolved by a process of natural selection primarily to regulate the amount of ultraviolet radiation penetrating the skin, controlling its biochemical effects. The actual skin color of different humans is affected by many substances, although the single most important substance is the pigment melanin. DNA Similarities.
Melanin is a broad term for a group of natural pigments found in most organisms. Melanin is produced through a multistage chemical process known as melanogenesis, where the oxidation of the amino acid tyrosine is followed by polymerization. The melanin pigments are produced in a specialized group of cells known as melanocytes. Grey Hair.
Melanogenesis is the process through which cells called melanocytes produce melanin. These cells develop in the neural tube of the foetus, then migrate to the underlying layer of the skin (the basal layer) before birth. Melanocytes also migrate to hair follicles and determine an individual’s hair colour. The process of melanin production is influenced by hormones, immune and inflammatory factors and brain signals.
Melanocytes interact with other skin cells called keratinocytes which are responsible for storing melanin in cells called melanosomes. Each melanocyte interacts with 30-40 keratinocytes to which it transfers melanin for storage in the skin’s layers until it is required for photo-protection (protecting the skin from UV radiation). In dark skinned individuals melanin is distributed throughout all the skin’s layers. It is stored for longer periods of time. In lighter skinned individuals melanin degradation occurs more quickly. The melanin which is produced is stored mainly in the upper layer of skin (the squamous cells) with very little melanin stored in the under layer of skin (the basal layer). In determining skin colour, the number melanocytes of is not as important as the type of melanin the cells produce. The number of melanin producing cells is similar between people of different ethnic groups. Hyper-pigmentation (e.g. as in darkening of the nipples during pregnancy) and hypo-pigmentation (as in albinism) occur without change in the number of melanocytes. It is the process of melanin production and the manner in which melanosomes are transferred to and distributed within keratinocytes which changes skin colour. The size and quantity of melanosomes, also determines skin colour. Darkly pigmented skin is associated with larger and more prolific melanosomes. They are elongated and the melanin they produce is stored in the keratinocytes for longer than it is stored in the keratinocytes of fair skinned individuals. In addition to melanin, other pigments including haemoglobin and carotene also help determine skin colour. Haemoglobin is a red pigment running along blood vessels. It results in skin being redder in places where the blood vessels come closer to the surface, for example the lips. Carotene is an orange/yellow pigment found in the skin as well as in yellow and orange vegetables. Eating excessive quantities of vegetables like carrots over a long period of time can change the skin colour. However it’s a rare occurrence and won’t happen with normal fruit and vegetable intake. If you notice your palms, face or the soles of your feet take on a yellow tinge, it’s far more likely to be a result of liver problems than it is eating too many carrots. Excess amounts of carotene can result in accumulation in the skin, concentrated in tissues containing fat, for example the skin yellowing associated with jaundice from liver dysfunction. The skin may also show abnormal colours such as: Cyanosis: Blueness of the skin in this condition occurs due to low levels of oxygen in the circulating blood. This deficiency causes the haemoglobin to turn reddish-violet. Erythema: refers to skin reddening and occurs due to increased blood flow in dilated blood vessels. Pallor: Loss of colour due to decreased blood flow. Exposure to the ultraviolet radiation from the sun causes changes to the skin colour. In the short term too much sun can result in what doctors called erythema and most people refer to as sunburn. Artificial exposure to UV radiation, for example from a tanning bed has a similar effect. In the longer term UV exposure stimulates melanin production causing skin reddening to change to darker, tanned skin within a few days. Other UV induced skin changes include thickening of the outer layer of skin, freckles and moles and premature skin ageing, characterised by reduced elasticity, increased dryness and wrinkles. Immediate skin changes (immediate pigmentation), seen within 5-10 minutes of sun exposure and lasting for minutes to several days, are induced by UVA radiation. They occur not because of increased melanin production but due to redistribution of melanin stored in keratinocytes in the upper layers of the skin. Delayed pigmentation which occurs several days after exposure to sunlight and has a longer duration (several weeks) is induced mainly by UVB radiation. These changes occur due to increasing production of melanin, particularly eumelanin. Over long periods of time, chronic sun exposure increases melanin levels and increased levels of eumelanin offer additional protection from the sun’s UV radiation. Exposure to UV radiation from the sun and artificial sources like tanning beds is a major risk factor for all types of skin cancer (melanoma, the rarest but most deadly type, basal cell carcinoma and squamous cell carcinoma). The duration and intensity of sun exposure influences the type of skin cancer. Chronic sun exposure, for example being exposed to the sun everyday due to outdoor work, influences the melanin content of the skin; over time skin darkens. Chronic sun exposure does not appear to increase, and may offer protection from melanoma. Intermittent, acute sun exposure is the major risk factor for melanoma, because over-exposure to sunlight causes cancerous DNA changes. Acute sun exposure refers to exposure for short periods of time in an individual whose skin is not usually exposed to the sun and is more likely to result in sunburn. This type of sun exposure occurs in office workers who spend a weekend or holiday at the beach. Skin type influences the risk of cancer. Darker skin with more melanin is less likely to burn and skin cancer is rarely seen in darkly pigmented individuals, except on the non-pigmented skin of their bodies like the soles of their feet and palms of their hands. Fair skinned patients are more susceptible to the acute effects of sun exposure and have a relatively high risk of skin Cancer. As skin cancer risk increases with cumulative lifetime exposure to UV radiation, age is also a risk factor. Skin cancer is not however limited to the adult population; 6% of all cancers in children are melanoma, which is the second most common form of cancer in 15-29 year olds.
Penn-led Study Identifies Genes Responsible for Diversity of Human Skin Colors - Diversity
How We Get Our Skin Color (youtube)
Body Image - Body Language - Body Smart Kinesthetic
Human skin comes in a wide variety of colours, ranging from shades of dark brown to almost white. Although an individual’s skin colour is influenced by numerous factors, the most significant is its content of a pigment called melanin. Melanin is also the pigment responsible for determining hair and eye colour. Levels of melanin are primarily determined by genetics; individuals born to fair skinned parents will inherit their parent’s fair skin, as individuals born to dark skinned parents will inherit dark skin. The level of inherited skin pigmentation is referred to as constitutive pigmentation. A number of other factors determined at birth, for example the way a person’s body produces hormones and the way these hormones signal the cells which produce melanin, also influence skin colour. These factors inherited at birth, which cannot be changed, are referred to as intrinsic factors. Skin type is a classification based on the skin’s reaction to exposure to the sun’s UV radiation, after a period of non-exposure (e.g. sun exposure at the beginning of summer, when the skin has not been exposed during winter). The skin’s reaction is measured in terms of burning and tanning. The Fitzpatrick system of classifying skin type is most commonly used in the assessment of skin cancer risk. The Fitzpatrick skin types are: Type I Extremely fair skin, always burns, never tans. Type II Fair skin, always burns, sometimes tans. Type III Medium skin, sometimes burns, always tans. Type IV Olive skin, rarely burns, always tans. Type V Moderately pigmented brown skin, never burns, always tans. Type VI Markedly pigmented black skin, never burns, always tans. Extrinsic factors, things outside the body, also influence skin colour and provide acquired pigmentation. Exposure to ultraviolet (UV) radiation from the sun is the most important extrinsic factor. The sun emits UVA and UVB rays and the different types of UV rays have different effects on skin pigmentation. Exposure to UVA rays produces immediate pigmentation by influencing melanin which has already been produced and is waiting in the skin’s upper layers. Pigmentation which occurs several days after sun exposure is a result of new melanin being produced in response to UVB exposure. Other extrinsic factors which influence skin pigmentation and colour include DNA damage (often induced by UVB exposure) and age, as the way the body produces melanin changes as a person ages. Skin colour is primarily determined by genetic inheritance but exposure to sunlight also alters skin colour. There are six skin types, fair skin that always burn, dark skin that never burns and everything in between. Melanin is the pigment that determines skin colour as well as hair and eye colour. Melanin is produced by skin cells when they are exposed to the sun. The more sun exposure, the more melanin is produced. There are two types of melanin, eumelanin which gives skin a brown colour (tan) and pheomelanin which gives skin a red colour (burn). Regular sun exposure (e.g. every day) is associated with tanning. It increases eumelanin levels which gives skin a brownish tan and provides protection against the sun’s rays. This reduces the risk of burning and skin cancer with future sun exposure. Irregular sun exposure (e.g. only during holidays or weekends) is associated with burning. It increases pheomelanin levels and increases cancer risk. Exposure to artificial ultra-violet radiation from tanning beds has the same effect on skin colour and cancer risk as exposure to the sun’s ultra violet rays.
Child Development - Human Development
Body Worlds - Anatomage Virtual Dissection
Stress - Heart Disease - Cancer - Immune System
Sunken Chest or pectus excavatum, is a congenital deformity of the anterior thoracic wall in which the sternum and rib cage grow abnormally. This produces a caved-in or sunken appearance of the chest. It can either be present at birth or not develop until puberty.
Deformity is a major abnormality in the shape of a body part or organ compared to the normal shape of that part. Deformity may arise from numerous causes: Genetic mutation. Damage to the fetus or uterus. Complications at birth. A growth or hormone disorder. Reconstructive surgery following a severe injury, e.g. burn injury. Arthritis and other rheumatoid disorders. Fractured bones left to heal without being properly set (malunion). Chronic application of external forces, e.g. artificial cranial deformation. Chronic paresis, paralysis or muscle imbalance, especially in children, e.g. due to poliomyelitis or cerebral palsy. Deformity can occur in non-humans, as well. Frogs can be mutated due to Ribeiroia (Trematoda) infection.
Gigantism is a condition characterized by excessive growth and height significantly above average. In humans, this condition is caused by over-production of growth hormone in childhood resulting in people between 7 feet (2.13 m) and 9 feet (2.75 m) in height.
Body Temperature
Body Temperature is a narrow temperature range indicating optimal health and thermoregulation. Individual body temperature depends upon the age, exertion, infection, sex, time of day, and reproductive status of the subject, the place in the body at which the measurement is made, the subject's state of consciousness (waking or sleeping), activity level, and emotional state. Despite these factors, typical values are well established: oral (under the tongue): 36.8±0.4 °C (98.2±0.72 °F), internal (rectal, vaginal): 37.0 °C (98.6 °F). Temperature measuring has several scales and units, the most common being Celsius (denoted °C; formerly called centigrade), Fahrenheit (denoted °F), and, especially in science, Kelvin (denoted K).
A decline in average body temperature among healthy adults over the past two decades. In the nearly two centuries since 98.6 degrees Fahrenheit or 37.0 degrees Celsius was established as the standard 'normal' body temperature. Declines might be due to lower rates of lingering mild infections or other factors. A 2017 study among 35,000 adults in the United Kingdom found average body temperature to be lower (97.9°F), and a 2019 study showed that the normal body temperature in Americans (those in Palo Alto, California, anyway) is about 97.5°F.
Fever (thermometers) - Heat (hot high temperatures) - Some People Feel Cold (youtube).
Thermoregulation is the ability of an organism to keep its body temperature within certain boundaries, even when the surrounding temperature is very different. A thermoconforming organism, by contrast, simply adopts the surrounding temperature as its own body temperature, thus avoiding the need for internal thermoregulation. The internal thermoregulation process is one aspect of homeostasis: a state of dynamic stability in an organism's internal conditions, maintained far from thermal equilibrium with its environment (the study of such processes in zoology has been called physiological ecology). If the body is unable to maintain a normal temperature and it increases significantly above normal, a condition known as hyperthermia occurs. For humans, this occurs when the body is exposed to constant temperatures of approximately 55 °C (131 °F), and with prolonged exposure (longer than a few hours) at this temperature and up to around 75 °C (167 °F) death is almost inevitable.[citation needed] Humans may also experience lethal hyperthermia when the wet bulb temperature is sustained above 35 °C (95 °F) for six hours. The opposite condition, when body temperature decreases below normal levels, is known as hypothermia.
Sweating - Heat Index - Wind Chill
Thermoception is the sense by which an organism perceives temperatures. The details of how temperature receptors work are still being investigated. Ciliopathy is associated with decreased ability to sense Heat, thus cilia may aid in the process. Transient receptor potential channels (TRP channels) are believed to play a role in many species in sensation of hot, cold, and pain. Mammals have at least two types of sensor: those that detect heat (i.e., temperatures above body temperature) and those that detect cold (i.e. temperatures below body temperature.
Thermographic Camera, also called an infrared camera or thermal imaging camera, is a device that forms an image using infrared radiation, similar to a common camera that forms an image using visible light. Instead of the 400–700 nanometre range of the visible light camera, infrared cameras operate in wavelengths as long as 14,000 nm (14 µm). Their use is called thermography. Temperature Sensors.
Homeothermy is thermoregulation that maintains a stable internal body temperature regardless of external influence. This internal body temperature is often, though not necessarily, higher than the immediate environment.
Warm-Blooded animal species can maintain a body temperature higher than their environment. In particular, homeothermic species maintain a stable body temperature by regulating metabolic processes. The only known homeotherms are birds and mammals. Other species have various degrees of thermoregulation. Hibernation - Ice.
Ectotherm is controlling body temperature through external metabolic processes, such as by basking in the sun. An organism in which internal physiological sources of heat are of relatively small or quite negligible importance in controlling body temperature.
Endotherm is an organism that maintains its body at a metabolically favorable temperature, largely by the use of heat set free by its internal bodily functions instead of relying almost purely on ambient heat. Such internally generated heat is mainly an incidental product of the animal's routine metabolism, but under conditions of excessive cold or low activity an endotherm might apply special mechanisms adapted specifically to heat production. Examples include special-function muscular exertion such as shivering, and uncoupled oxidative metabolism such as within brown adipose tissue. Only birds and mammals are extant universally endothermic groups of animals. Certain lamnid sharks, tuna and billfishes are also endothermic.In common parlance, endotherms are characterized as "warm-blooded". The opposite of endothermy is ectothermy, although there is no absolute or clear separation between the nature of endotherms and ectotherms in general.
Poikilotherm is the ability of an organism to function over a wide internal temperature range. An animal whose internal temperature varies considerably. Usually the variation is a consequence of variation in the ambient environmental temperature. Many terrestrial ectotherms are poikilothermic. However some ectotherms remain in temperature-constant environments to the point that they are actually able to maintain a constant internal temperature (i.e. are homeothermic). It is this distinction that often makes the term "poikilotherm" more useful than the vernacular "cold-blooded", which is sometimes used to refer to ectotherms more generally. Poikilothermic animals include types of vertebrate animals, specifically fish, amphibians, and reptiles, as well as a large number of invertebrate animals. The naked mole-rat is the only mammal that is currently thought to be poikilothermic.
Bradymetabolism is the ability to greatly alter metabolic rate in response to need; for example, animals that hibernate. Organisms with a high active metabolism and a considerably slower resting metabolism. Bradymetabolic animals can often undergo dramatic changes in metabolic speed, according to food availability and temperature. Many bradymetabolic creatures in deserts and in areas that experience extreme winters are capable of "shutting down" their metabolisms to approach near-death states, until favorable conditions return. Several variants of bradymetabolism exists. In mammals, the animals normally have a fairly high metabolism, only dropping to low levels in times of little food. In most reptiles, the normal metabolic rate is quite low, but can be raised when needed, typically in short bursts of activity in connection with capturing prey. Hibernation.
Ice Therapy
Vasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood vessels. The process is particularly important in staunching hemorrhage and acute blood loss. When blood vessels constrict, the flow of blood is restricted or decreased, thus retaining body heat or increasing vascular resistance. This makes the skin turn paler because less blood reaches the surface, reducing the radiation of heat. On a larger level, vasoconstriction is one mechanism by which the body regulates and maintains mean arterial pressure.
Mitochondrial Disease is a group of disorders caused by dysfunctional mitochondria, the organelles that generate energy for the cell. Mitochondria are found in every cell of the human body except red blood cells, and convert the energy of food molecules into the ATP that powers most cell functions.
Underactive-Thyroid
Hypothyroidism is a common disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goitre. Untreated hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby, which is called cretinism.
Winter Camping
Targeted Temperature Management was previously known as therapeutic hypothermia or protective hypothermia is active treatment that tries to achieve and maintain a specific body temperature in a person for a specific duration of time in an effort to improve health outcomes during recovery after a period of stopped blood flow to the brain. This is done in an attempt to reduce the risk of tissue injury following lack of blood flow. Periods of poor blood flow may be due to cardiac arrest or the blockage of an artery by a clot as in the case of a stroke. Targeted temperature management improves survival and brain function following resuscitation from cardiac arrest. Evidence supports its use following certain types of cardiac arrest in which an individual does not regain consciousness. Both 33 °C (91 °F) and 36 °C (97 °F) appear to result in similar outcomes. Targeted temperature management following traumatic brain injury has shown mixed results with some studies showing benefits in survival and brain function while others show no clear benefit. While associated with some complications, these are generally mild. Targeted temperature management is thought to prevent brain injury by several methods including decreasing the brain's oxygen demand, reducing the production of neurotransmitters like glutamate, as well as reducing free radicals that might damage the brain. The lowering of body temperature may be accomplished by many means including the use of cooling blankets, cooling helmets, cooling catheters, ice packs and ice water lavage.
Hyperthermia is elevated body temperature due to failed thermoregulation that occurs when a body produces or absorbs more heat than it dissipates. Extreme temperature elevation then becomes a medical emergency requiring immediate treatment to prevent disability or death. The most common causes include heat stroke and adverse reactions to drugs. The former is an acute temperature elevation caused by exposure to excessive heat, or combination of heat and humidity, that overwhelms the heat-regulating mechanisms. The latter is a relatively rare side effect of many drugs, particularly those that affect the central nervous system. Malignant hyperthermia is a rare complication of some types of general anesthesia. Hyperthermia differs from fever in that the body's temperature set point remains unchanged. The opposite is hypothermia, which occurs when the temperature drops below that required to maintain normal metabolism. The term is from Greek υπε, ype, meaning "excess", and θερμία, thermía, meaning "heat". Wim Hof - How to Survive a Fall Through Ice.
Hyperthermic conditioning is a scientific term for what happens to your body, when you're exposed to very hot conditions like a sauna. When you sit in a sauna, your body goes through several physiological changes: It increases plasma volume, which is a good thing because it improves blood flow to the heart. Hyperthermic conditioning has been shown to reduce muscle glycogen use by 40%-50% compared to before heat acclimation. Adaptation.
Hyperthermic Conditioning for Hypertrophy, Endurance, and Neurogenesis (youtube)
Sauna is a small room or building designed as a place to experience heat temperatures approaching and exceeding 100 °C (212 °F), which would be completely intolerable and possibly fatal if exposed to long periods of time. Saunas overcome this problem by controlling the humidity. A steam sauna can take 30 minutes to heat up when first started. Some users prefer taking a warm shower beforehand to speed up perspiration in the sauna. When in the sauna users often sit on a towel for hygiene and put a towel over the head if the face feels too hot but the body feels comfortable. In Russia, a felt "banya hat" may be worn to shield the head from the heat; this allows the wearer to increase the heat on the rest of the body. Most adjustment of temperature in a sauna comes from, amount of water thrown on the heater, this increases humidity, so that sauna bathers perspire more copiously. length of stay in the sauna positioning when in the sauna.
IGF 1 or insulin-like growth factor 1, is a protein that in humans is encoded by the IGF1 gene. IGF-1 has also been referred to as a "sulfation factor" and its effects were termed "nonsuppressible insulin-like activity" (NSILA) in the 1970s. IGF-1 is a hormone similar in molecular structure to insulin. It plays an important role in childhood growth and continues to have anabolic effects in adults. A synthetic analog of IGF-1, mecasermin, is used for the treatment of growth failure. IGF-1 consists of 70 amino acids in a single chain with three intramolecular disulfide bridges. IGF-1 has a molecular weight of 7,649 Daltons.
Heat Acclimation is a broad term that can be loosely defined as a complex series of changes or adaptations that occur in response to heat stress in a controlled environment over the course of 7 to 14 days. These adaptations are beneficial to exercise in the heat and allow the body to better cope with Heat Stress.
Heat Shock Protein 32 as a novel survival factor and therapeutic target in neoplastic mast cells. (Hsp32).
Occupational Heat Stress is when workers who are exposed to extreme heat or work in hot environments may be at risk of heat stress. Exposure to extreme heat can result in occupational illnesses and injuries. Heat stress can result in heat stroke, heat exhaustion, heat cramps, or heat rashes.
Heat Stroke is a severe heat illness, defined as hyperthermia with a body temperature greater than 40.6 °C (105.1 °F) because of environmental heat exposure with lack of thermoregulation. This is distinct from a fever, where there is a physiological increase in the temperature set point of the body. The term "stroke" in "heat stroke" is a misnomer in that it does not involve a blockage or hemorrhage of blood flow to the brain. Preventive measures include drinking plenty of cool liquids and avoiding excessive heat and humidity, especially in unventilated spaces, such as parked cars, that can overheat quickly. Treatment requires rapid physical cooling of the body. First Aid.
Heat Shock is the effect of subjecting a cell to a higher temperature than that of the ideal body temperature of the organism from which the cell line was derived. Heat shock refers to the cellular exposure to rapid changes in stressors such as temperature, toxins, oxidative stress, heavy metals, and pathogenic infections. Specifically temperature induced heat shock, even by a change of a few degrees, causes proteins to misfold, nonspecifically aggregate, and/or entangle. Other cellular damage induced by heat shock includes cytoskeleton rearrangement, changes in organelle localization, decreased ATP production, drop in cellular pH, decreased translation, and changes in RNA splicing. Introduction of heat shock to cells elicits the molecular response, the heat shock response (HSR), which repairs damages caused by stressors such as protein misfolding and protein aggregation.
Hypothermia is reduced body temperature that happens when a body dissipates more heat than it absorbs. In humans, it is defined as a body core temperature below 35.0 °C (95.0 °F). Symptoms depend on the temperature. In mild hypothermia there is shivering and mental confusion. In moderate hypothermia shivering stops and confusion increases. In severe hypothermia there may be paradoxical undressing, in which a person removes his or her clothing, as well as an increased risk of the heart stopping. Hypothermia has two main types of causes. It classically occurs from exposure to extreme cold. It may also occur from any condition that decreases heat production or increases heat loss. Commonly this includes alcohol intoxication but may also include low blood sugar, anorexia, and advanced age, among others. Body temperature is usually maintained near a constant level of 36.5–37.5 °C (97.7–99.5 °F) through thermoregulation. Efforts to increase body temperature involve shivering, increased voluntary activity, and putting on warmer clothing. Hypothermia may be diagnosed based on either a person's symptoms in the presence of risk factors or by measuring a person's core temperature. The treatment of mild hypothermia involves warm drinks, warm clothing and physical activity. In those with moderate hypothermia heating blankets and warmed intravenous fluids are recommended. People with moderate or severe hypothermia should be moved gently. In severe hypothermia extracorporeal membrane oxygenation (ECMO) or cardiopulmonary bypass may be useful. In those without a pulse cardiopulmonary resuscitation (CPR) is indicated along with the above measures. Rewarming is typically continued until a person's temperature is greater than 32 °C (90 °F). If there is no improvement at this point or the blood potassium level is greater than 12 mmol/liter at any time resuscitation may be discontinued. Hypothermia is the cause of at least 1,500 deaths a year in the United States. It is more common in older people and males. One of the lowest documented body temperatures from which someone with accidental hypothermia has survived is 13.0 °C (55.4 °F) in a near-drowning of a 7-year-old girl in Sweden. Survival after more than six hours of CPR has been described. In those in whom ECMO or bypass is used survival is around 50%. Deaths due to hypothermia have played an important role in many wars. Hyperthermia is the opposite of hypothermia, being an increased body temperature due to failed thermoregulation. The term is from Greek ὑπο, ypo, meaning "under", and θερμία, thermía, meaning "heat".
Heat Escape Lessening Position is a way to position oneself to reduce heat loss while immersed in cold water. It is taught as part of the curriculum in Australia, North America, and Ireland for lifeguard and boating safety training. It involves essentially positioning one's knees together and hugging them close to the chest using one's arms. Furthermore, groups of people can huddle together in this position to conserve body heat, offer moral support, and provide a larger target for rescuers. The HELP is an attempt to reduce heat loss enough to lessen the effect of hypothermia. Hypothermia is essentially a condition where bodily temperature drops too low to perform normal voluntary or involuntary functions. Cold water causes "immersion hypothermia", which can cause damage to extremities or the body's core, including unconsciousness or death. The HELP reduces exposure of high heat loss areas of the body. Wearing a personal flotation device allows a person to draw their knees to their chest and arms to their sides, while still remaining able to breathe.
Endothermic Process describes a process or reaction in which the system absorbs energy from its surroundings; usually, but not always, in the form of heat. The term was coined by Marcellin Berthelot from the Greek roots endo-, derived from the word "endon" meaning "within" and the root "therm" meaning "hot." The intended sense is that of a reaction that depends on absorbing heat if it is to proceed. The opposite of an endothermic process is an exothermic process, one that releases, "gives out" energy in the form of heat. Thus in each term (endothermic & exothermic) the prefix refers to where heat goes as the reaction occurs, though in reality it only refers to where the energy goes, without necessarily being in the form of heat.
Sleeping Temperature - Warm Clothing
Infrared Heater or heat lamp, is a body with a higher temperature which transfers energy to a body with a lower temperature through electromagnetic radiation. Depending on the temperature of the emitting body, the wavelength of the peak of the infrared radiation ranges from 780 nm to 1 mm. No contact or medium between the two bodies is needed for the energy transfer. Infrared heaters can be operated in vacuum or atmosphere. One classification of infrared heaters is by the wavelength bands of infrared emission. Short wave or near infrared for the range from 780 nm to 1400 nm, these emitters are also named bright because still some visible light is emitted; Medium infrared for the range between 1400 nm and 3000 nm; Far infrared or dark emitters for everything above 3000 nm.
Ice Ice Baby
Hydrotherapy is a part of medicine and alternative medicine, in particular of naturopathy, occupational therapy and physiotherapy, that involves the use of water for pain relief and treatment. The term encompasses a broad range of approaches and therapeutic methods that take advantage of the physical properties of water, such as temperature and pressure, for therapeutic purposes, to stimulate blood circulation and treat the symptoms of certain diseases. Various therapies used in the present-day hydrotherapy employ water jets, underwater massage and mineral baths (e.g. balneotherapy, Iodine-Grine therapy, Kneipp treatments, Scotch hose, Swiss shower, thalassotherapy) and/or whirlpool bath, hot Roman bath, hot tub, Jacuzzi, cold plunge and mineral bath. Water has Memory.
Cold Shower for Health - Syncope (dizzy fainting)
Ice Bath Therapy is a training regimen usually following a period of intense exercise in which a substantial part of a human body is immersed in a bath of ice or ice-water for a limited duration. While it is becoming increasingly popular and accepted among athletes in a variety of sports, the method is controversial, with a risk of hypothermia, with the possibility of shock leading to sudden death. Many athletes have used cold water immersion after an intense exercise workout on the belief that it speeds up bodily recovery; however, the internal physical processes are not well understood and remain elusive. Generally research into the health effects of cold water immersion as part of an athletic training regimen is inconclusive, with some studies suggesting a mild benefit such as reducing muscle damage and discomfort and alleviating delayed onset muscle soreness, with other studies suggesting that cold water immersion may slow muscle growth and interfere with an overall training regimen. Ice Bath.
Breathing - Thin Ice 2.0: Weight Loss Clothing thermogenic calorie burning.
Thalassotherapy is the use of seawater as a form of therapy. It is based on the systematic use of seawater, sea products, and shore climate. The properties of seawater are believed to have beneficial effects upon the pores of the skin.
Balneotherapy may involve hot or cold water, massage through moving water, relaxation, or stimulation. Many mineral waters at spas are rich in particular minerals such as silica, sulfur, selenium, and radium. Medicinal clays are also widely used, a practice known as 'fangotherapy. Weather Changes.
Frozen in Time
Cryotherapy is the local or general use of low temperatures in medical therapy. Cryotherapy is used to treat a variety of benign and malignant tissue damage, medically called lesions. Kryo Life Health.
Cryonics is the low-temperature preservation (usually at −196°C) of people who cannot be sustained by contemporary medicine, with the hope that resuscitation and restoration to full health may be possible in the far future. Cryopreservation of humans is not reversible with present technology; cryonicists hope that medical advances will someday allow cryopreserved people to be revived. Seeds - Dormancy.
Embryo Cryopreservation is the process of preserving an embryo at sub-zero temperatures, generally at an embryogenesis stage corresponding to pre-implantation, that is, from fertilisation to the blastocyst stage.
Semen Cryopreservation is a procedure to preserve sperm cells. Semen can be used successfully indefinitely after cryopreservation. For human sperm, the longest reported successful storage is 24 years. It can be used for sperm donation where the recipient wants the treatment in a different time or place, or as a means of preserving fertility for men undergoing vasectomy or treatments that may compromise their fertility, such as chemotherapy, radiation therapy or surgery.
Cryogenics is the study of the production and behaviour of materials at very low temperatures. Ice.
Hibernation is a state of inactivity and metabolic depression in endotherms. Hibernation refers to a season of heterothermy that is characterized by low body temperature, slow breathing and heart rate, and low metabolic rate. Although traditionally reserved for "deep" hibernators such as rodents, the term has been redefined to include animals such as bears and is now applied based on active metabolic suppression rather than based on absolute body temperature decline. Many experts believe that the processes of daily torpor and hibernation form a continuum and utilize similar mechanisms. The equivalent during the summer months is known as aestivation. Some reptile species (ectotherms) are said to brumate, or undergo brumation, but any possible similarities between brumation and hibernation are not firmly established. Some insects, such as the wasp Polistes exclamans, hibernate by aggregating together in groups in protected places called hibernacula.
Insect Winter Ecology entails the overwinter survival strategies of insects, which are in many respects more similar to those of plants than to many other animals, such as mammals and birds. This is because unlike those animals, which can generate their own heat internally (endothermic), insects must rely on external sources to provide their heat (ectothermic). Thus, insects sticking around in the winter, must tolerate freezing or rely on other mechanisms to avoid freezing. Loss of enzymatic function and eventual freezing due to low temperatures daily threatens the livelihood of these organisms during winter. Not surprisingly, insects have evolved a number of strategies to deal with the rigors of winter temperatures in places where they would otherwise not survive.
Antarctic Flies protect Fragile Eggs with 'Antifreeze'. Temperature-resistant gel helps the eggs of wingless flies survive the extreme conditions of the southern continent.
Emergency Preservation and Resuscitation normovolemic cardiac arrest in pigs.
Cryptobiosis is an ametabolic state of life entered by an organism in response to adverse environmental conditions such as desiccation, freezing, and oxygen deficiency. In the cryptobiotic state, all measurable metabolic processes stop, preventing reproduction, development, and repair. When environmental conditions return to being hospitable, the organism will return to its metabolic state of life as it was prior to the cryptobiosis.
Cryobiology is the branch of biology that studies the effects of low temperatures on living things within Earth's cryosphere or in science. In practice, cryobiology is the study of biological material or systems at temperatures below normal. Materials or systems studied may include proteins, cells, tissues, organs, or whole organisms. Temperatures may range from moderately hypothermic conditions to cryogenic temperatures.
Physical Therapy
Physical Therapy is used to improve a patient's quality of life through examination, consultation, research, education, diagnosis, prognosis and physical intervention using mechanical force, movements, manual therapy and exercise therapy to promote mobility, function and reduce pain. Physical therapy attempts to address the illnesses, or injuries that limit a person's abilities to move and perform functional activities in their daily lives. PTs use an individual's history and physical examination to arrive at a diagnosis and establish a management plan and, when necessary, incorporate the results of laboratory and imaging studies like X-rays, CT-scan, or MRI findings. Electrodiagnostic testing (e.g., electromyograms and nerve conduction velocity testing) may also be used. PT management commonly includes prescription of or assistance with specific exercises, manual therapy and manipulation, mechanical devices such as traction, education, physical agents which includes heat, cold, electricity, sound waves, radiation, assistive devices, prostheses, orthoses and other interventions. In addition, PTs work with individuals to prevent the loss of mobility before it occurs by developing fitness and wellness-oriented programs for healthier and more active lifestyles, providing services to individuals and populations to develop, maintain and restore maximum movement and functional ability throughout the lifespan. This includes providing therapeutic treatment in circumstances where movement and function are threatened by aging, injury, disease or environmental factors. Functional movement is central to what it means to be healthy. (performed by physical therapists, known as physiotherapists, physiotherapy). Caregiving.
Physical Therapy - Physical Therapy News - Physical Therapy Journal
Message - Posture (back & neck) - Sports Medicine
"Physical therapy is like braces for your teeth, you have to keep doing it in order to receive the benefits and make progress. But you also need to know when to change things or modify things because you can make things worse."
Occupational Therapy is the use of assessment and treatment to develop, recover, or maintain the daily living and work skills of people with a physical, mental, or cognitive disorder. Occupational Therapists also focus much of their work on identifying and eliminating environmental barriers to independence and participation in daily activities. Occupational therapists work with clients of all ages, ranging from infants to the elderly. Occupational therapy interventions focus on adapting the environment, modifying the task, teaching the skill, and educating the client/family in order to increase participation in and performance of daily activities, particularly those that are meaningful to the client. Occupational therapists often work closely with professionals in physical therapy, speech therapy, nursing, social work, and the community. Occupational Therapy.
Physical Rehabilitation is a branch of medicine that aims to enhance and restore functional ability and quality of life to those with physical impairments or disabilities. A physician having completed training in this field is referred to as a physiatrist. Physiatrists specialize in restoring optimal function to people with injuries to the muscles, bones, ligaments, or nervous system.
Sports Medicine - Water Therapy
Physical Therapy Game (video)
Heat Therapy is the use of heat in therapy, such as for pain relief and health. It can take the form of a hot cloth, hot water bottle, ultrasound, heating pad, hydrocollator packs, whirlpool baths, cordless FIR heat therapy wraps, and others. It can be beneficial to those with arthritis and stiff muscles and injuries to the deep tissue of the skin. Heat may be an effective self-care treatment for conditions like rheumatoid arthritis. Heat therapy is most commonly used for rehabilitation purposes. The therapeutic effects of heat include increasing the extensibility of collagen tissues; decreasing joint stiffness; reducing pain; relieving muscle spasms; reducing inflammation, edema, and aids in the post acute phase of healing; and increasing blood flow. The increased blood flow to the affected area provides proteins, nutrients, and oxygen for better healing. Body Temp.
Broken Bones (first aid)
Related Subjects - Stem Cells - Cells - DNA - Genetic Testing - Biology - Water - Body Smart - Meditation - Brain - Plasticity - Blood Brain Barrier - Metabolism - Inflammation - Hygiene - Teeth - Dentistry - Skin - Sweat - Bathing - Cold Shower - Nails - Hands - Feet - Hair - Pee - Urine - Poo - Human Faeces - Bowl Movement.
Pain
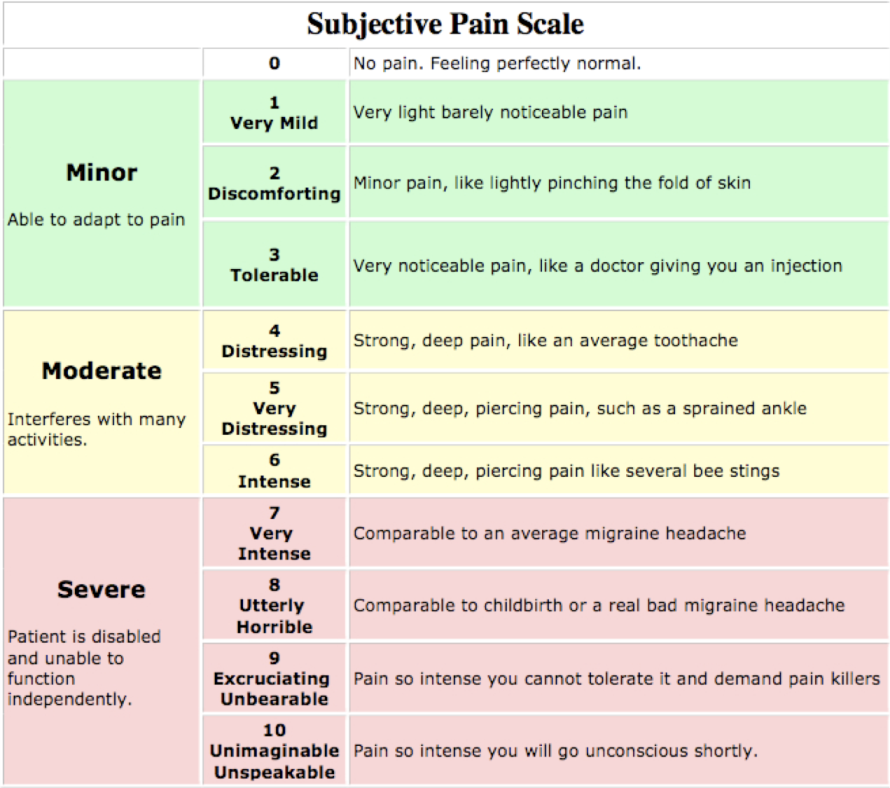 Pain
is a natural response to
help us avoid injury to the body. It is a
distressing feeling often caused by intense or damaging
stimuli, such as
stubbing a toe, burning a finger,
putting alcohol on a cut, or bumping the "funny bone". Pain is an
unpleasant sensory and
emotional experience associated with actual or potential tissue damage, or
described in terms of such damage.
Pain
is a natural response to
help us avoid injury to the body. It is a
distressing feeling often caused by intense or damaging
stimuli, such as
stubbing a toe, burning a finger,
putting alcohol on a cut, or bumping the "funny bone". Pain is an
unpleasant sensory and
emotional experience associated with actual or potential tissue damage, or
described in terms of such damage.Pain Scale measures a patient's pain intensity or other features. Pain scales are based on self-report, observational (behavioral), or physiological data. Self-report is considered primary and should be obtained if possible. Pain scales are available for neonates, infants, children, adolescents, adults, seniors, and persons whose communication is impaired. Pain assessments are often regarded as "The 5th Vital Sign".
Excruciating is something that is extremely painful that can torment you emotionally or mentally, like being tortured.
Ouch is a word that is used to express a feeling of pain.
Hurt is to feel physical or mental pain and have a source of pain. Any physical damage to the body caused by an injury, violence, accident or fracture etc.. Cause damage or affect negatively. Cause emotional anguish or make miserable. Psychological suffering.
Senses (body smart) - Back Pain (posture) - People Who Can't Feel Pain
Threshold of Pain is the point along a curve of increasing perception of a stimulus at which pain begins to be felt. It is an entirely subjective phenomenon. A distinction must be maintained between the stimulus (an external thing that can be directly measured, such as with a thermometer) and the person or animal's resulting pain perception (an internal, subjective thing that can sometimes be measured indirectly, such as with a visual analog scale). Although an IASP document defines "pain threshold" as "the minimum intensity of a stimulus that is perceived as painful". Kratom.
Detection: Acute pain begins with nociceptors—long neurons that originate in the spinal cord and end as thin fibers in the skin. Those fibers are tipped with receptors that respond to pain-inducing stimuli. When a stimulus is strong enough, these receptors generate an electrical current—the pain signal.
Transmission: The pain signal travels along the neurons through a series of channels that allow sodium ions back and forth across cell membranes. These channels, like Nav1.7, allow those charged particles across a membrane if the pain signal is strong enough. (If it isn’t, the person feels no pain.)
Perception: When a pain signal reaches the spinal cord, it continues up to the brain, where the somatosensory cortex is primarily responsible for translating information about the intensity of the pain signal. The brain’s motor cortex then generates the body’s response—a shout of surprise, a jerk of a hand.
Aftermath: After an injury, even an innocuous stimulus—like a warm bath or a pat on the back—can generate a pain signal at the site of the original injury.
Nociceptor is a sensory nerve cell that responds to damaging or potentially damaging stimuli by sending signals to the spinal cord and brain. This process, called nociception, usually causes the sensation of pain in sentient beings. (nociceptive glio-neural complex). Nociceptor Sensory Neuron-Immune Interactions in Pain and Inflammation.
Nociception is the sensory nervous system's response to certain harmful or potentially harmful stimuli by sending “possible threat” signals to the spinal cord and the brain. If the brain perceives the threat as credible, it creates the sensation of pain to direct attention to the body part, so the threat can hopefully be mitigated; this process is called nociception. (nociceptive glio-neural complex).. In nociception, intense chemical (e.g., chili powder in the eyes), mechanical (e.g., cutting, crushing), or thermal (heat and cold) stimulation of sensory nerve cells called nociceptors produces a signal that travels along a chain of nerve fibers via the spinal cord to the brain. Nociception triggers a variety of physiological and behavioral responses and usually results in a subjective experience of pain in sentient beings.
Thermal Comfort is the condition of mind that expresses satisfaction with the thermal environment and is assessed by subjective evaluation (ANSI/ASHRAE Standard 55). Maintaining this standard of thermal comfort for occupants of buildings or other enclosures is one of the important goals of HVAC (heating, ventilation, and air conditioning) design engineers.
Cold Compression Therapy also known as hilotherapy, combines two of the principles of rest, ice, compression, elevation to reduce pain and swelling from a sports or activity injury to soft tissues and recommended by orthopedic surgeons following surgery. The therapy is especially useful for sprains, strains, pulled muscles and pulled ligaments.
Weather Pains - Tooth Pain - Processed Food (msg)
Soreness is a pain that is felt (as when the area is touched). An uncomfortable feeling of mental painfulness or distress.
Neuropathic Pain is pain caused by damage or disease affecting the somatosensory nervous system. Neuropathic pain may be associated with abnormal sensations called dysesthesia or pain from normally non-painful stimuli (allodynia). It may have continuous and/or episodic (paroxysmal) components. The latter resemble stabbings or electric shocks. Common qualities include burning or coldness, "pins and needles" sensations, numbness and itching.
Psychological Pain or mental pain is an unpleasant feeling and suffering of a psychological, non-physical, origin. Resilience.
Visceral Pain is pain that results from the activation of nociceptors of the thoracic, pelvic, or abdominal viscera (organs). Visceral structures are highly sensitive to distension (stretch), ischemia and inflammation, but relatively insensitive to other stimuli that normally evoke pain such as cutting or burning. Visceral pain is diffuse, difficult to localize and often referred to a distant, usually superficial, structure. It may be accompanied by symptoms such as nausea, vomiting, changes in vital signs as well as emotional manifestations. The pain may be described as sickening, deep, squeezing, and dull. Distinct structural lesions or biochemical abnormalities explain this type of pain in only a proportion of patients. These diseases are grouped under gastrointestinal neuromuscular diseases (GINMD). Others can experience occasional visceral pains, often very intense in nature, without any evidence of structural, biochemical or histolopathologic reason for such symptoms. These diseases are grouped under functional gastrointestinal disorders (FGID) and the pathophysiology and treatment can vary greatly from GINMD. The two major single entities among functional disorders of the gut are functional dyspepsia and irritable bowel syndrome. Visceral hypersensitivity is hypersensitive visceral pain perception, which is commonly experienced by individuals with functional gastrointestinal disorders.
Arthritis is a disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types other organs are also affected. Onset can be gradual or sudden. Arthritis Foundation.
Sciatica is a medical condition characterized by pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes but not always present. Weakness or numbness may occur in various parts of the affected leg and foot. Sciatic Nerve is a large nerve in humans and animals. It begins in the lower back and runs through the buttock and down the lower limb. It is the longest and widest single nerve in the human body, going from the top of the leg to the foot on the posterior aspect. The sciatic nerve provides the connection to the nervous system for nearly the whole of the skin of the leg, the muscles of the back of the thigh, and those of the leg and foot. It is derived from spinal nerves L4 to S3. It contains fibers from both the anterior and posterior divisions of the lumbosacral plexus.
Chronic Pain is pain that lasts a long time. In medicine, the distinction between acute and chronic pain is sometimes determined by an arbitrary interval of time since onset; the two most commonly used markers being 3 months and 6 months since onset.
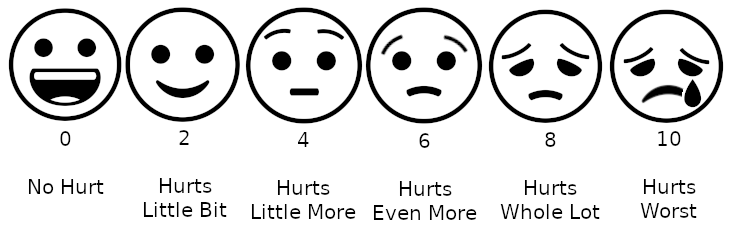 Partners Against Pain
Partners Against Pain
Secret World Of Pain (youtube)
Elliot Krane: Chronic Pain (video)
Strong Painkiller Ketamine Reaction | Scotland's Superhospital (youtube)
Headache is the symptom of pain anywhere in the region of the head or neck. It occurs in migraines (sharp, or throbbing pains), tension-type headaches, and cluster headaches. Frequent headaches can affect relationships and employment. There is also an increased risk of depression in those with severe headaches.
Migraine is a primary headache disorder characterized by recurrent headaches that are moderate to severe. Typically, the headaches affect one half of the head, are pulsating in nature, and last from two to 72 hours. Associated symptoms may include nausea, vomiting, and sensitivity to light, sound, or smell. The pain is generally made worse by physical activity. Up to one-third of people have an aura: typically a short period of visual disturbance that signals that the headache will soon occur. Occasionally, an aura can occur with little or no headache following it.
Thunderclap Headache is a headache that is severe and sudden-onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. It can be indicative of a number of medical problems, most importantly subarachnoid hemorrhage, which can be life-threatening. Usually, further investigations are performed to identify the underlying cause.
A combination of physical and occupational therapy, massage and nutrition counseling can be more effective than just pain medication. Exercise, rehabilitation therapies, yoga and cognitive behavioral therapies and cognitive behavioral therapy can be used to help relieve pain. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016.
The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Chronic pain-induced depression. In particular, injury sensory pathways of body pains have been shown to share the same brain regions involved in mood management, including the insular cortex, prefrontal cortex, anterior cingulate, thalamus, hippocampus, and amygdala, which form a histological structural foundation for the coexistence of pain and depression . Furthermore, the volumes of the prefrontal cortex (PFC) and hippocampus have been reported in many studies to be significantly smaller in depressed patients and to be closely related to depression severity. In addition, individuals with depression in postmortem studies have also been observed to have a significantly reduced number of PFC synapses, which thus decreases synaptic functions. Meanwhile, the effect of PFC on pain development via the nucleus accumbens has also been verified, thus indicating that the occurrence and development of pain and depression may be associated with some identical neuroplasticity changes. Furthermore, maladaptive plasticity changes, which refer to the plasticity in the nervous system that leads to a disruption of the function and may be considered a disease state, have also been indicated in a large number of clinical trials and animal studies. Additionally, these maladaptive plasticity changes may also occur in sensory conduction pathways from the peripheral to the central nervous system and participate in the occurrence, development, and maintenance of chronic pain . In summary, chronic pain and depression may be based on common neuroplasticity mechanism changes, which are a potentially important route for the onset and aggravation of chronic pain and depression. Reviewing the role of neuroplasticity in chronic pain and depression, this paper explores the influence of analgesic drugs and antidepressants with different pharmacological effects on neuroplasticity as well as their contribution to individualized application strategies in the treatment of chronic pain-induced depression. Monoamine neurotransmitters, including serotonin (5-HT), dopamine (DA), and norepinephrine (NE), have been studied in molecular mechanisms involved in chronic pain and depression.Glutamate functions as one of the main excitatory neurotransmitters in the CNS and exists in synapses throughout the brain . Furthermore, glutamate and its receptor subtypes, N-methyl-D-aspartic acid (NMDA) receptor and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, have been found to be involved in the occurrence and development of chronic pain and depression. In the spinal cord, both increased excitatory system activity and the accompanying reduced inhibitory system are known to contribute to central hyperalgesia and to ultimately lead to the progression of pathological pain . Glutamatergic activity can be promoted through the breakdown of efficient inhibition of the actions of glutamate by GABA.
Prostaglandin are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. They are derived enzymatically from the fatty acid arachidonic acid. Every prostaglandin contains 20 carbon atoms, including a 5-carbon ring. They are a subclass of eicosanoids and of the prostanoid class of fatty acid derivatives. Prostaglandins are powerful locally acting vasodilators and inhibit the aggregation of blood platelets. Through their role in vasodilation, prostaglandins are also involved in inflammation. They are synthesized in the walls of blood vessels and serve the physiological function of preventing needless clot formation, as well as regulating the contraction of smooth muscle tissue. Prostaglandins are produced following the sequential oxygenation of arachidonic acid, DGLA or EPA by cyclooxygenases (COX-1 and COX-2) and terminal prostaglandin synthases. The classic dogma is as follows: COX-1 is responsible for the baseline levels of prostaglandins. COX-2 produces prostaglandins through stimulation. However, while COX-1 and COX-2 are both located in the blood vessels, stomach and the kidneys, prostaglandin levels are increased by COX-2 in scenarios of inflammation and growth.
Arachidonic Acid is a polyunsaturated omega-6 fatty acid involved in cellular signaling as a lipid second messenger involved in the regulation of signaling enzymes, such as PLC-γ, PLC-δ, and PKC-α, -β, and -γ isoforms, arachidonic acid is a key inflammatory intermediate and can also act as a vasodilator.
Periaqueductal Gray is the primary control center for descending pain modulation. It has enkephalin-producing cells that suppress pain. The periaqueductal gray is the gray matter located around the cerebral aqueduct within the tegmentum of the midbrain. It projects to the nucleus raphe magnus, and also contains descending autonomic tracts. The ascending pain and temperature fibers of the spinothalamic tract send information to the PAG via the spinomesencephalic tract (so-named because the fibers originate in the spine and terminate in the PAG, in the mesencephalon or midbrain). This region has been used as the target for brain-stimulating implants in patients with chronic pain. Stimulation of the periaqueductal gray matter of the midbrain activates enkephalin-releasing neurons that project to the raphe nuclei in the brainstem. 5-HT (serotonin) released from the raphe nuclei descends to the dorsal horn of the spinal cord where it forms excitatory connections with the "inhibitory interneurons" located in Laminae II (aka the substantia gelatinosa). When activated, these interneurons release either enkephalin or dynorphin (endogenous opioid neurotransmitters), which bind to mu opioid receptors on the axons of incoming C and A-delta fibers carrying pain signals from nociceptors activated in the periphery. The activation of the mu-opioid receptor inhibits the release of substance P from these incoming first-order neurons and, in turn, inhibits the activation of the second-order neuron that is responsible for transmitting the pain signal up the spinothalamic tract to the ventroposteriolateral nucleus (VPL) of the thalamus. The nociceptive signal was inhibited before it was able to reach the cortical areas that interpret the signal as "pain" (such as the anterior cingulate). This is sometimes referred to as the Gate control theory of pain and is supported by the fact that electrical stimulation of the PAG results in immediate and profound analgesia. The periaqueductal gray is also activated by viewing distressing images associated with pain. Three known kinds of opioid receptors have been identified: mu (μ), kappa (κ) and delta (δ). Synthetic opioid and opioid-derivative drugs activate these receptors (possibly by acting on the PAG directly, where these receptors are densely expressed) to produce analgesia. These drugs include morphine, heroin (diacetylmorphine), pethidine, hydrocodone, oxycodone, and similar pain-reducing compounds.
Cutaneous Nerve is a nerve that innervates the skin, responsible for providing sensory innervation to the skin.
Pinched Nerve (body smart) - Posture
Nerve Compression Syndrome is a medical condition caused by direct pressure on a nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression (by a herniated disc, for example). Its symptoms include pain, tingling, numbness and muscle weakness.
Radiculopathy refers to a set of conditions in which one or more nerves are affected and do not work properly (a neuropathy). The location of the injury is at the level of the nerve root (radix = "root"). This can result in pain (radicular pain), weakness, numbness, or difficulty controlling specific muscles.
Peripheral Neuropathy is damage to or disease affecting nerves, which may impair sensation, movement, gland or organ function, or other aspects of health, depending on the type of nerve affected. Common causes include systemic diseases (such as diabetes or leprosy), vitamin deficiency, medication (e.g., chemotherapy, or commonly prescribed antibiotics including Metronidazole and the Fluoroquinolone class of antibiotics (Ciprofloxacin, Levaquin, Avelox etc.)), traumatic injury, radiation therapy, excessive alcohol consumption, immune system disease, Coeliac disease, or viral infection.
Familial Dysautonomia is a disorder of the autonomic nervous system which affects the development and survival of sensory, sympathetic and some parasympathetic neurons in the autonomic and sensory nervous system resulting in variable symptoms, including insensitivity to pain, inability to produce tears, poor growth, and labile blood pressure (episodic hypertension and postural hypotension).
Human Insula particularly its posterior portion, is often regarded as a primary cortex for pain.
Somatic Nervous System is the part of the peripheral nervous system associated with skeletal muscle voluntary control of body movements. The SoNS consists of afferent nerves and efferent nerves. Afferent nerves are responsible for relaying sensation from the body to the central nervous system (CNS); efferent nerves are responsible for sending out commands from the CNS to the body, stimulating muscle contraction; they include all the non-sensory neurons connected with skeletal muscles and skin. The a- of afferent and the e- of efferent correspond to the prefixes ad- (to, toward) and ex- (out of).
Scientists find the Amygdala can be Pain-Suppression Circuit. People do believe there is a central place to relieve pain, that's why placebos work. general anesthesia promotes slow-wave sleep by activating the supraoptic nucleus of the brain. The researchers found that general anesthesia also activates a specific subset of inhibitory neurons in the central amygdala, which they have called the CeAga neurons (CeA stands for central amygdala; ga indicates activation by general anesthesia).
Autonomic Nervous System is a division of the peripheral nervous system that influences the function of internal organs. The autonomic nervous system is a control system that acts largely unconsciously and regulates bodily functions such as the heart rate, digestion, respiratory rate, pupillary response, urination, and sexual arousal. This system is the primary mechanism in control of the fight-or-flight response and the freeze-and-dissociate response.
Opioid Receptor are a group of inhibitory G protein-coupled receptors with opioids as ligands. The endogenous opioids are dynorphins, enkephalins, endorphins, endomorphins and nociceptin. The opioid receptors are ~40% identical to somatostatin receptors (SSTRs). Opioid receptors are distributed widely in the brain, and are found in the spinal cord and digestive tract.
Opioid System controls pain, reward and addictive behaviors. Opioid receptors in the brain are activated by a family of endogenous peptides like enkephalins, dynorphins and endorphin, which are released by neurons. Endogeny (wiki) - Kratom.
Opioid Antagonist is a receptor antagonist that acts on one or more of the opioid receptors. Naloxone and naltrexone are commonly used opioid antagonist drugs which are competitive antagonists that bind to the opioid receptors with higher affinity than agonists but do not activate the receptors. This effectively blocks the receptor, preventing the body from responding to opioids and endorphins.
Opiate is a drug derived from opium. Opioid is found naturally in a number of plants and animals. A more modern term for Opiate is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain.
Mu opioid receptor: a gateway to drug addiction. Mu opioid receptors mediate positive reinforcement following direct (morphine) or indirect (alcohol, cannabinoids, nicotine) activation, and our understanding of mu receptor function is central to the development of addiction therapies. Recent data obtained in native neurons confirm that mu receptor signaling and regulation are strongly agonist-dependent. Current functional mapping reveals morphine-activated neurons in the extended amygdala and early genomic approaches have identified novel mu receptor-associated proteins. A classification of about 30 genes either promoting or counteracting the addictive properties of morphine is proposed from the analysis of knockout mice data. The targeting of effectors or regulatory proteins, beyond the mu receptor itself, might provide valuable strategies to treat addictive disorders.
The endogenous opioid system and clinical pain management. The endogenous opioid system is one of the most studied innate pain-relieving systems. This system consists of widely scattered neurons that produce three opioids: beta-endorphin, the met- and leu-enkephalins, and the dynorphins. These opioids act as neurotransmitters and neuromodulators at three major classes of receptors, termed mu, delta, and kappa, and produce analgesia. Like their endogenous counterparts, the opioid drugs, or opiates, act at these same receptors to produce both analgesia and undesirable side effects. This article examines some of the recent findings about the opioid system, including interactions with other neurotransmitters, the location and existence of receptor subtypes, and how this information drives the search for better analgesics. We also consider how an understanding of the opioid system affects clinical responses to opiate administration and what the future may hold for improved pain relief. The goal of this article is to assist clinicians to develop pharmacological interventions that better meet their patient's analgesic needs.
μ-opioid receptor are a class of opioid receptors with a high affinity for enkephalins and beta-endorphin, but a low affinity for dynorphins. They are also referred to as μ-opioid peptide (MOP) receptors. The prototypical μ-opioid receptor agonist is morphine, the primary psychoactive alkaloid in opium. It is an inhibitory G-protein coupled receptor that activates the Gi alpha subunit, inhibiting adenylate cyclase activity, lowering cAMP levels.
Fighting opioids with an unlikely supplemental painkiller: Anti-itch medicine that targets a specific part of our nerve cells that can make morphine.
Dynorphin are a class of opioid peptides that arise from the precursor protein prodynorphin. When prodynorphin is cleaved during processing by proprotein convertase 2 (PC2), multiple active peptides are released: dynorphin A, dynorphin B, and α/β-neo-endorphin. Depolarization of a neuron containing prodynorphin stimulates PC2 processing, which occurs within synaptic vesicles in the presynaptic terminal. Occasionally, prodynorphin is not fully processed, leading to the release of “big dynorphin.” This 32-amino acid molecule consists of both dynorphin A and dynorphin B. Dynorphin A, dynorphin B, and big dynorphin all contain a high proportion of basic amino acid residues, in particular lysine and arginine (29.4%, 23.1%, and 31.2% basic residues, respectively), as well as many hydrophobic residues (41.2%, 30.8%, and 34.4% hydrophobic residues, respectively). Although dynorphins are found widely distributed in the CNS, they have the highest concentrations in the hypothalamus, medulla, pons, midbrain, and spinal cord. Dynorphins are stored in large (80-120 nm diameter) dense-core vesicles that are considerably larger than vesicles storing neurotransmitters. These large dense-core vesicles differ from small synaptic vesicles in that a more intense and prolonged stimulus is needed to cause the large vesicles to release their contents into the synaptic cleft. Dense-core vesicle storage is characteristic of opioid peptides storage. The first clues to the functionality of dynorphins came from Goldstein et al. in their work with opioid peptides. The group discovered an endogenous opioid peptide in the porcine pituitary that proved difficult to isolate. By sequencing the first 13 amino acids of the peptide, they created a synthetic version of the peptide with a similar potency to the natural peptide. Goldstein et al. applied the synthetic peptide to the guinea ileum longitudinal muscle and found it to be an extraordinarily potent opioid peptide. The peptide was called dynorphin (from the Greek dynamis=power) to describe its potency. Dynorphins exert their effects primarily through the κ-opioid receptor (KOR), a G-protein-coupled receptor. Two subtypes of KORs have been identified: K1 and K2. Although KOR is the primary receptor for all dynorphins, the peptides do have some affinity for the μ-opioid receptor (MOR), δ-opioid receptor (DOR), and the N-methyl-D-aspartic acid (NMDA)-type glutamate receptor. Different dynorphins show different receptor selectivities and potencies at receptors. Big dynorphin and dynorphin A have the same selectivity for human KOR, but dynorphin A is more selective for KOR over MOR and DOR than is big dynorphin. Big dynorphin is more potent at KORs than is dynorphin A. Both big dynorphin and dynorphin A are more potent and more selective than dynorphin B.
Hydromorphone is an opioid agonist that binds to several opioid receptors. Its analgesic characteristics are through its effect on the mu-opioid receptors. It also acts centrally at the level medulla, depressing the respiratory drive and suppressing cough. Hydromorphone is a Narcotic that can treat moderate to severe pain and a Controlled substance with High risk for addiction and dependence. Can cause respiratory distress and death when taken in high doses or when combined with other substances, especially alcohol. Hydromorphone is also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is an opioid used to treat moderate to severe pain. Typically, long-term use is only recommended for pain due to cancer. It may be used by mouth or by injection into a vein, muscle, or under the skin. Effects generally begin within half an hour and last for up to five hours.
Pharmacological Extinction or Pharmacological enhancement of drug cue extinction learning: translational challenges.
Endogenous is having an internal cause or origin. Growing or originating from within an organism.
Endorphins are produced by the central nervous system and the pituitary gland with a principal function to inhibit the transmission of pain signals; they may also produce a feeling of euphoria very similar to that produced by other Opioids, which are substances that act on opioid receptors to produce morphine-like effects. Opioids act by binding to opioid receptors, which are found principally in the central and peripheral nervous system and the gastrointestinal tract.
Wearable Pain Relief (Quell)
LumiWave: Pain Relief is now In-Demand!
Livia - The Off Switch for Menstrual Pain
PAT- home use device that treats the underlying cause of pain.
iTENS Device - Wireless Electrotherapy
Spinal Stimulation - Nervo HF10
Stellate Ganglion Block is an injection of medication into these nerves that can help relieve pain in the head, neck, upper arm and upper chest. A stellate ganglion block is used to diagnose or treat circulation problems or nerve injuries, including: Reflex sympathetic dystrophy.
Trigeminal Neuralgia is a chronic pain disorder that affects the largest of the cranial nerves, the Trigeminal Nerve, which is a nerve responsible for sensation in the face and motor functions such as biting and chewing. Cranial Nerves are the nerves that emerge directly from the brain (including the brainstem), in contrast to spinal nerves (which emerge from segments of the spinal cord). Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck. There are two main types: typical and atypical trigeminal neuralgia. The typical form results in episodes of severe, sudden, shock like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face. Both forms may occur in the same person. It is one of the most painful conditions and can result in depression. The exact cause is unclear but believed to involve loss of the myelin around the trigeminal nerve. This may occur due to compression from a blood vessel as the nerve exits the brain stem, multiple sclerosis, stroke, or trauma. Less common causes include a tumor or arteriovenous malformation. It is a type of nerve pain. Diagnosis is typically based on the symptoms after ruling out other possible causes such as postherpetic neuralgia. Treatment includes medication or surgery. The anticonvulsant carbamazepine or oxcarbazepine is the usual initial treatment and is effective in about 80% of people. Other options include lamotrigine, baclofen, gabapentin, and pimozide. Amitriptyline may help with the pain but opioids are not usually effective in the typical form. In those who do not improve or become resistant to other measures, a number of types of surgery may be tried.
Fibromyalgia is a medical condition characterised by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems, and troubles with memory. Some people also report restless legs syndrome, bowel or bladder problems, numbness and tingling, and sensitivity to noise, lights or temperature. Fibromyalgia is frequently associated with depression, anxiety, and posttraumatic stress disorder. Other types of chronic pain are also frequently present.
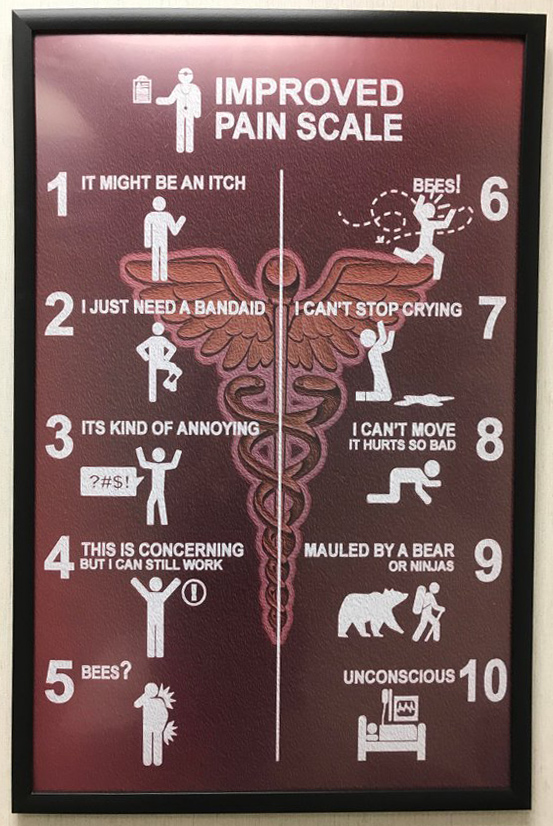 Pain Psychologist works as part of a multidisciplinary pain treatment
team within an academic pain clinic, private pain clinic, in a hospital
rehabilitation setting, or in an outpatient chronic pain functional
restoration program. The plan often involves teaching relaxation
techniques, changing old beliefs about pain, building new coping skills
and addressing any anxiety or depression that may accompany your pain.
Pain Psychologist works as part of a multidisciplinary pain treatment
team within an academic pain clinic, private pain clinic, in a hospital
rehabilitation setting, or in an outpatient chronic pain functional
restoration program. The plan often involves teaching relaxation
techniques, changing old beliefs about pain, building new coping skills
and addressing any anxiety or depression that may accompany your pain.
Prospect for more effective treatment of nerve pain.
Painkillers without Dangerous Side Effects
Sex Differences in Brain Activity Alter Pain Therapies.
Certain exercises can help manage pain, with mineral supplements.
BetterBack Therapy.
Cells carry 'memory' of injury.
Pain Rehabilitation Center Bio-Psychosocial Approach.
Brain's insular cortex processes pain and drives learning from pain.
Evaluation of Group and Individual Change in a Multidisciplinary Pain Management Program
Pain Management Programs (American Chronic Pain Association).
Chronic Pain Program (Medical Advanced Pain Specialist Medical Pain Clinics).
Ketorolac Toradol is a non-steroidal anti-inflammatory drug (NSAID) in the family of heterocyclic acetic acid derivatives, used as an analgesic, which is any member of the group of drugs used to achieve analgesia, relief from pain.
Feverfew is a traditional medicinal herb which is commonly used to prevent migraine headaches, and is also occasionally grown for ornament.
Petasites is a genus of flowering plants in the sunflower family, Asteraceae.
Congenital Insensitivity is one or more rare conditions in which a person cannot feel (and has never felt) physical pain.
Anesthetic is a drug to prevent pain during surgery, completely blocking any feeling as opposed to an Analgesic. A wide variety of drugs are used in modern anesthetic practice.
Analgesic is any member of the group of drugs used to achieve analgesia, relief from pain. Analgesic drugs act in various ways on the peripheral and central nervous systems. They are distinct from anesthetics, which temporarily affect, and in some instances completely eliminate, sensation. Analgesics include paracetamol (known in North America as acetaminophen or simply APAP), the nonsteroidal anti-inflammatory drugs (NSAIDs) such as the salicylates, and opioid drugs such as morphine and oxycodone. Half-Asleep - Psychedelics - Time Perception.
Analgesia is the absence of the sense of pain without loss of consciousness.
Green Light Therapy is a Drug-Free Idea To Relieve Chronic Pain - Light-Induced Analgesia
Anesthesia is a state of temporary induced loss of sensation or awareness. It may include analgesia or the relief from or prevention of pain, paralysis or muscle relaxation, amnesia or the loss of memory, or unconsciousness. A patient under the effects of anesthetic drugs is referred to as being anesthetized. Anesthesia enables the painless performance of medical procedures that would cause severe or intolerable pain to an unanesthetized patient. Three broad categories of anaesthesia exist: General anesthesia suppresses central nervous system activity and results in unconsciousness and total lack of sensation. Sedation suppresses the central nervous system to a lesser degree, inhibiting both anxiety and creation of long-term memories without resulting in unconsciousness. Regional anesthesia and local anesthesia, which block transmission of nerve impulses between a targeted part of the body and the central nervous system, causing loss of sensation in the targeted body part. A patient under regional or local anesthesia remains conscious, unless general anaesthesia or sedation is administered at the same time. Two broad classes exist: Peripheral blockade inhibits sensory perception in an isolated part of the body, such as numbing a tooth for dental work or administering a nerve block to inhibit sensation in an entire limb. Central, or neuraxial, blockade administers the anesthetic in the region of the central nervous system itself, suppressing incoming sensation from outside the area of the block. Examples include epidural anaesthesia and spinal anaesthesia.
Anesthesiology is the medical speciality concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialised in this field of medicine is called an anesthesiologist, anaesthesiologist or anaesthetist, depending on the country. The core element of the specialty is the study and use of anesthesia and anesthetics to safely support a patient's vital functions through the perioperative period.
I Can't Feel Anything - People who Feel No Pain
Numbness is partial or total lack of sensation in a part of the body; a symptom of nerve damage or dysfunction. Not Happy or Sad.
Paralysis is loss of muscle function for one or more muscles. Paralysis accompanied by a loss of feeling or sensory loss in the affected area if there is sensory damage as well as motor. About 1 in 50 people in the U.S. have been diagnosed with some form of paralysis, transient or permanent.
Brain Injuries - Stroke - Coma - Sleep Paralysis
Paresthesia is an abnormal sensation of the skin (tingling, pricking, chilling, burning, numbness) with no apparent physical cause. Paresthesia may be transient or chronic, and may have any of dozens of possible underlying causes. Paresthesias are usually painless and can occur anywhere on the body, but most commonly occur in the arms and legs. The most familiar kind of paresthesia is the sensation known as "pins and needles" after having a limb 'fall asleep'. A less well-known and uncommon but important paresthesia is formication, the sensation of insects crawling underneath the skin.
Spinal Cord Injury is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete injury, with a total loss of sensation and muscle function, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis to incontinence. Long term outcomes also ranges widely, from full recovery to permanent tetraplegia (also called quadriplegia) or paraplegia. Complications can include muscle atrophy, pressure sores, infections, and breathing problems.
Researchers restore breathing, partial forelimb function in rats with spinal cord injuries. Millions of people worldwide are living with chronic spinal cord injuries, with 250,000 to 500,000 new cases each year -- most from vehicle crashes or falls. The most severe spinal cord injuries completely paralyze their victims and more than half impair a person's ability to breathe. Now, a breakthrough study has demonstrated, in animal models of chronic injury, that long-term, devastating effects of spinal cord trauma on breathing and limb function may be reversible.
Designer cytokine makes paralyzed mice walk again. Using gene therapy, a research team has succeeded in getting mice to walk again after a complete cross-sectional injury. The nerve cells produced the curative protein themselves. To date, paralysis resulting from spinal cord damage has been irreparable. With a new therapeutic approach, scientists have succeeded for the first time in getting paralyzed mice to walk again. The keys to this are the protein hyper-interleukin-6, which stimulates nerve cells to regenerate, and the way it is supplied to the animals. Spinal cord injuries caused by sports or traffic accidents often result in permanent disabilities such as paraplegia. This is caused by damage to nerve fibers, so-called axons, which carry information from the brain to the muscles and back from the skin and muscles. If these fibers are damaged due to injury or illness, this communication is interrupted. Since severed axons in the spinal cord can't grow back, the patients suffer from paralysis and numbness for life. To date, there are still no treatment options that could restore the lost functions in affected patients. Cytokine are a broad and loose category of small proteins (~5–20 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrine, paracrine and endocrine signaling as immunomodulating agents. Their definite distinction from hormones is still part of ongoing research.
Re-Growing Damaged Nerves hinges on shutting down key Genes. Injured neurons temporarily revert to immature state. Neurons in the brain and spinal cord don't grow back after injury, unlike those in the rest of the body. About 11,000 people in the United States survive a spinal cord injury every year. The idea that cells must become less mature in order to regenerate is not new. The researchers identified the key molecular and genetic players involved in regressing to a less mature state, and showed that the timing of the regression was crucial to successful recovery.
Nerve transfers to restore upper limb function in tetraplegia. Nerve transfer surgery has enabled 13 young adults with complete paralysis to regain movement and function in their elbows and hands, according to the largest case series of this technique in people with tetraplegia (paralysis of both the upper and lower limbs).
Paraplegia is an impairment in motor or sensory function of the lower extremities.
Tetraplegia is paralysis caused by illness or injury that results in the partial or total loss of use of all four limbs and torso; paraplegia is similar but does not affect the arms. The loss is usually sensory and motor, which means that both sensation and control are lost. Tetraparesis or quadriparesis, on the other hand, means muscle weakness affecting all four limbs. It may be flaccid or spastic.
Micro implants could restore standing and walking. Researchers are focused on restoring lower-body function after severe spinal injuries using a tiny spinal implant.
Waterloo's Dr. Spine, Stuart McGill (youtube) Stuart McGill is one of the world's foremost experts on spine biomechanics.
Woman with Novel Gene Mutation lives almost Pain-Free. She also experiences very little anxiety and fear, and may have enhanced wound healing due to the mutation. Fatty Acid Amide Hydrolase is a member of the serine hydrolase family of enzymes.
Congenital Insensitivity to Pain is one or more rare conditions in which a person cannot feel and has never felt physical pain. The conditions described here are separate from the HSAN group of disorders, which have more specific signs and cause. Because feeling physical pain is vital for survival, CIP is an extremely dangerous condition. It is common for people with the condition to die in childhood due to injuries or illnesses going unnoticed. Burn injuries are among the more common injuries. (also known as congenital analgesia).
Fatigue
Fatigue is exhaustion, tiredness, languidness, languor, lassitude, and listlessness. Sometimes a subjective feeling of tiredness which is distinct from weakness, and has a gradual onset. Unlike weakness, fatigue can be alleviated by periods of rest. Fatigue can have physical or mental causes. Food Energy - Stamina.
Physical Fatigue is the transient inability of a muscle to maintain optimal physical performance, and is made more severe by intense physical exercise.
Mental Fatigue is a transient decrease in maximal cognitive performance resulting from prolonged periods of cognitive activity. It can manifest as somnolence, lethargy, or directed attention fatigue.
Tired is in need of Sleep or Rest and Feeling weary, but Not Lazy.
Weary is being physically and mentally fatigued and exhausted or tired from overuse or great strain or stress. Weary can also mean to lose interest or become bored with something or somebody.
Exhausted is being drained of energy or depleted of energy, force, or strength.
Exhaustion is a state of extreme physical or mental fatigue. The action or state of using something up or of being used up completely.
Depleted is no longer sufficient.
Drained is exhausted or very tired or emptied of liquid or electrical charge.
Incapacitated is someone lacking in or deprived of strength or power. Make unable to perform a certain action. Injured.
Lethargic is being sluggish and apathetic. Being affected by lethargy.
Lethargy is a state of tiredness, weariness, fatigue, or lack of energy. It can be accompanied by depression, decreased motivation, or apathy. Lethargy can be a normal response to inadequate sleep, overexertion, overworking, stress, lack of exercise, improper nutrition, boredom, or a symptom of a disorder. It may also be a side-effect of medication or caused by an interaction between medications or medication(s) and alcohol. When part of a normal response, lethargy often resolves with rest, adequate sleep, decreased stress, physical exercise and good nutrition.
Vegetative Symptoms are disturbances of a person's functions necessary to maintain life.
Weakness is a symptom of a number of different conditions. The causes are many and can be divided into conditions that have true or perceived muscle weakness. True muscle weakness is a primary symptom of a variety of skeletal muscle diseases, including muscular dystrophy and inflammatory myopathy. It occurs in neuromuscular junction disorders, such as myasthenia gravis.
Chronic Fatigue Syndrome or Myalgic Encephalomyelitis, is a medical condition characterized by long-term fatigue and other symptoms that limit a person's ability to carry out ordinary daily activities. Low levels of thyroid hormones are linked to chronic fatigue syndrome.
What happens when you have a disease doctors can't diagnose: Jennifer Brea (video and interactive text)
Stanford researchers have linked ME/CFS to variations in certain cytokines, immune-signaling proteins, that track with illness severity.
Things that may cause Fatigue: Poor nutrition or electrolyte imbalances, such as abnormal levels of sodium, potassium, calcium, and magnesium. Anemia, an abnormally low level of red blood cells. Sleep disturbances. Emotional distress, such as anxiety or depression. Medication side effects. Medical conditions, such as heart, lung, or hormone problems. Exposure to toxins. Environmental Pollution.
Researchers have turned a fungus into a disease-curing factory through modern genetic engineering and patience.
The natural antibiotic is a promising cure for a neglected tropical disease called human African trypanosomiasis, or African sleeping sickness, that infects thousands of people in remote, rural areas of sub-Saharan Africa each year. The fungus Acremonium egyptiacum naturally produces two different types of antibiotic: one is toxic to humans, but the other was identified as a potential treatment for African sleeping sickness. The fungus's two antibiotics are both made from the same precursor molecule. After the precursor is created, two separate groups of enzymes produce the two different antibiotics. Researchers can leave the precursor molecule and the genes responsible for the desired antibiotic completely unchanged by simply deleting the genes responsible for the other toxic antibiotic. In every liter of fungus that researchers grow in the lab, the engineered strain of the fungus can produce 500 milligrams of antibiotic. People can develop African sleeping sickness by being bitten by a fly. The disease is caused by a parasite that moves from the flies, to patients' blood streams, and then into the nerves of patients' brains and spinal cords. The disease is often fatal within three years. The same parasite can also infect livestock animals.
Tetraplegia also known as quadriplegia, is paralysis caused by illness or injury that results in the partial or total loss of use of all four limbs and torso; paraplegia is similar but does not affect the arms. The loss is usually sensory and motor, which means that both sensation and control are lost. Tetraparesis or quadriparesis, on the other hand, means muscle weakness affecting all four limbs. It may be flaccid or spastic.
Neural mechanisms and areas of the human brain that contribute to fatigue in people with depression, multiple sclerosis and stroke.
Things that may alleviate fatigue: Exercise, good sleep habits, eating well, and living with purpose, just to name a few.
Sitting to Long (sedentary) - Physical Therapy
No Spring Chicken is to describe someone who is no longer young and probably past their young adulthood, and sometimes doesn't realize it and tries to look and act younger than his age. This expression is a euphemism for calling someone old. Specifically, people mean that they are past the prime of their young adult years. Where the term came from. Chicks need to be raised in light, warm conditions, and in the past, it was not possible to create these special conditions like we do nowadays, so it was not possible for chicks to be raised in the winter. Farmers soon realized that chickens born in the spring were the most desirable at markets and buyers would pay the most for them. Farmers would often try to sell an older chicken pretending that it was born in the spring but smart buyers would say, “that’s no spring chicken!”
Endurance - Stamina - Strength
Physical Strength is the measure of an animal's exertion of force on physical objects. Increasing physical strength is the goal of strength training. An individual's physical strength is determined by two factors; the cross-sectional area of muscle fibers recruited to generate force and the intensity of the recruitment. Individuals with a high proportion of type I slow twitch muscle fibers will be relatively weaker than a similar individual with a high proportion of type II fast twitch fibers, but would have a greater inherent capacity for physical endurance. The genetic inheritance of muscle fiber type sets the outermost boundaries of physical strength possible (barring the use of enhancing agents such as testosterone), though the unique position within this envelope is determined by training. Individual muscle fiber ratios can be determined through a muscle biopsy. Other considerations are the ability to recruit muscle fibers for a particular activity, joint angles, and the length of each limb. For a given cross-section, shorter limbs are able to lift more weight. The ability to gain muscle also varies person to person, based mainly upon genes dictating the amounts of hormones secreted, but also on sex, age, health of the person, and adequate nutrients in the diet. A one-repetition maximum test is the most accurate way to determine maximum muscular strength. Food Energy.
Stamina is having enduring strength and energy and the ability to sustain prolonged physical or mental effort. Fatigue.
Endurance is the ability of an organism to exert itself and remain active for a long period of time, as well as its ability to resist, withstand, recover from, and have immunity to trauma, wounds, or fatigue. It is usually used in aerobic or anaerobic exercise. The definition of 'long' varies according to the type of exertion – minutes for high intensity anaerobic exercise, hours or days for low intensity aerobic exercise. Training for endurance can have a negative impact on the ability to exert strength unless an individual also undertakes resistance training to counteract this effect. When a person is able to accomplish or withstand a higher amount of effort than their original capabilities their endurance is increasing which to many personnel indicates progress. In looking to improve ones endurance they may slowly increase the amount of repetitions or time spent, if higher repetitions are taken rapidly muscle strength improves while less endurance is gained. Increasing endurance has been proven to release endorphins resulting in a positive mind. The act of gaining endurance through physical activity has been shown to decrease anxiety, depression, and stress, or any chronic disease in total. Although a greater endurance can assist the cardiovascular system it does not imply that any cardiovascular disease can be guaranteed to improve. "The major metabolic consequences of the adaptations of muscle to endurance exercise are a slower utilization of muscle glycogen and blood glucose, a greater reliance on fat oxidation, and less lactate production during exercise of a given intensity." The term stamina is sometimes used synonymously and interchangeably with endurance. In military settings, endurance is considered the ability of a force to sustain high levels of combat potential relative to its opponent over the duration of a campaign. Endurance may also refer to an ability to keep going through a tough situation involving hardship, stress, etc. (see patience).
Endurance Training is the act of exercising to increase endurance. The term endurance training generally refers to training the aerobic system as opposed to the anaerobic system. The need for endurance in sports is often predicated as the need of cardiovascular and simple muscular endurance, but the issue of endurance is far more complex. Endurance can be divided into two categories including: general endurance and specific endurance. It can be shown that endurance in sport is closely tied to the execution of skill and technique. A well conditioned athlete can be defined as, the athlete who executes his or her technique consistently and effectively with the least effort. Key for measuring endurance are heart rate, power in cycling and pace in running.
Limit to Human Endurance. Everyone hits the same metabolic limit, likely due to constraints on the digestive tract's ability to break down food. Humans can only burn calories at 2.5 times their resting metabolic rate. Not even the world's fastest ultra-marathoners managed to surpass that limit. The body starts to break down its own tissues to make up for the caloric deficit.
Posture - Sit Up Straight
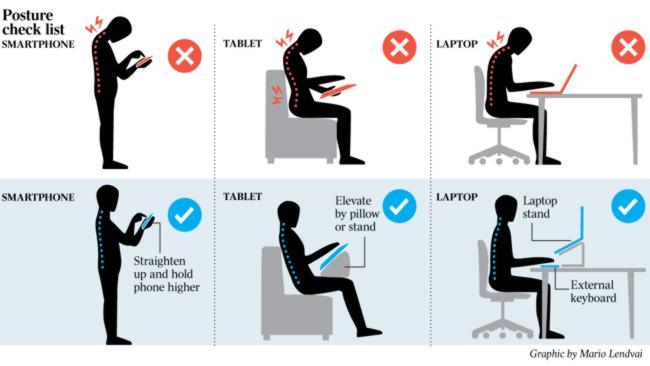 Posture is the position in which you hold
your body upright against gravity while standing, sitting or lying down.
Good posture involves training your body to stand, walk, sit and lie in
positions where the least strain is placed on supporting
muscles and
ligaments during movement or weight-bearing activities.
Posture is the position in which you hold
your body upright against gravity while standing, sitting or lying down.
Good posture involves training your body to stand, walk, sit and lie in
positions where the least strain is placed on supporting
muscles and
ligaments during movement or weight-bearing activities.Improve Posture (youtube)
Improve Your Posture | 3 Exercises Only! (youtube)
Good Posture - Balance Center
Text Neck (smartphones) - Spine Disases
Poor Posture is the posture that results from certain muscles tightening up or shortening while others lengthen and become weak which often occurs as a result of one's daily activities. There are different factors which can impact on posture and they include occupational activities and biomechanical factors such as force and repetition. Risk factors for poor posture also include psychosocial factors such as job stress and strain. Workers who have higher job stress are more likely to develop neck and shoulder symptoms.
Lumbar Support helps promote good posture by filling in the gap between the lumbar spine and the seat, supporting the natural inward curve of the lower back. Lumbar is the abdominal segment of the torso, between the diaphragm and the sacrum. Sometimes referred to as the lower spine, or as an area of the back in its proximity. Car Seat is made from inexpensive but durable material in order to withstand prolonged use but you may still need some lumbar support. I like to use a rolled up towel and place it near my lower back when I sit in a chair or sit on a couch. You have to figure out how to place the towel where it will have the most benefit, you also need to adjust the way you roll up the towel, tight or loss. "This is lumbar support, how can I help you?" Physical Therapy.
Ergonomics is known as comfort design, functional design, and systems, is the practice of designing products, systems, or processes to take proper account of the interaction between them and the people who use them. Human Factors Ergonomics field has seen some contributions from numerous disciplines, such as psychology, engineering, biomechanics, industrial design, physiology, and anthropometry. In essence, it is the study of designing equipment, devices and processes that fit the human body and its cognitive abilities. The two terms "human factors" and "ergonomics" are essentially synonymous.
Anthropometry refers to the measurement of the human individual for the purposes of understanding human physical variation, in paleoanthropology and in various attempts to correlate physical with racial and psychological traits. Anthropometry involves the systematic measurement of the physical properties of the human body, primarily dimensional descriptors of body size and shape.
Fitts Law is a predictive model of human movement primarily used in human–computer interaction and ergonomics. This scientific law predicts that the time required to rapidly move to a target area is a function of the ratio between the distance to the target and the width of the target. Fitts's law is used to model the act of pointing, either by physically touching an object with a hand or finger, or virtually, by pointing to an object on a computer monitor using a pointing device. Fitts's law has been shown to apply under a variety of conditions, with many different limbs (hands, feet, the lower lip, head-mounted sights, eye gaze), manipulanda (input devices), physical environments (including underwater), and user populations (young, old, special educational needs, and drugged participants).
Alexander Technique is an educational process that develops the ability to realign posture and to avoid unnecessary muscular and mental tension. Alexander believed the individual's self-awareness could be inaccurate, resulting in unnecessary muscular tension such as when standing or sitting with body weight unevenly distributed, holding one's head incorrectly, walking or running inefficiently, and responding to stressful stimuli in an exaggerated way. Alexander said that those who habitually "misused" their muscles could not trust their feelings (sensory appreciation) when carrying out activities or responding to situations emotionally.
Neutral Spine refers to the "three natural curves [that] are present in a healthy spine." Looking directly at the front or back of the body, the 33 vertebrae in the spinal column should appear completely vertical. From a side view, the cervical (neck) region of the spine (C1-C7) is bent inward, the thoracic (upper back) region (T1-T12) bends outward, and the lumbar (lower back) region (L1-L5) bends inward. The sacrum (tailbone area) (S1-S5 fused) and coccyx (on average 4 fused) rest between the pelvic bones. A neutral pelvis indicates the anterior superior iliac spines and pubic symphysis fall in the same vertical line.
Human Positions refers to the different physical configurations that the human body can take. There are several synonyms that refer to human positioning, often used interchangeably, but having specific nuances of meaning. Position is a general term for a configuration of the human body. Posture means an intentionally or habitually assumed position. Pose implies artistic or aesthetic intention of the position. Attitude refers to postures assumed for purpose of imitation, intentional or not, as well as in some standard collocations in reference to some distinguished types of posture: "Freud never assumed a fencer's attitude, yet almost all took him for a swordsman." Bearing refers to the manner of the posture, as well as of gestures and other aspects of the conduct taking place. Sleeping Positions
Flexion is the anatomical name for forward bending. When treating back pain, many spine specialists encourage exercises to strengthen the muscles that act to bring the spine into flexion. In the lower back, approximately 50% of flexion occurs at the hips, and 50% occurs at the lower spine. Motion is divided between the five motion segments in the lower back, although a disproportionate amount of the motion is at L4-L5 (lumbar segment 4 and 5) and L3-L4 (lumbar segment 3 and 4). Consequently, these two segments of the lower back are the most likely to break down and become unstable from osteoarthritis (degenerative spondylolisthesis), with an excess of motion creating low back pain. Yoga.
Thoracic Vertebrae compose the middle segment of the vertebral column, between the cervical vertebrae and the lumbar vertebrae. In humans, there are twelve thoracic vertebrae and they are intermediate in size between the cervical and lumbar vertebrae; they increase in size going towards the lumbar vertebrae, with the lower ones being a lot larger than the upper. They are distinguished by the presence of facets on the sides of the bodies for articulation with the heads of the ribs, as well as facets on the transverse processes of all, except the eleventh and twelfth, for articulation with the tubercles of the ribs. By convention, the human thoracic vertebrae are numbered T1–T12, with the first one (T1) located closest to the skull and the others going down the spine toward the lumbar region. Spine Health.
How to Fix Your Posture in 4 Moves! (PERMANENTLY) (youtube)
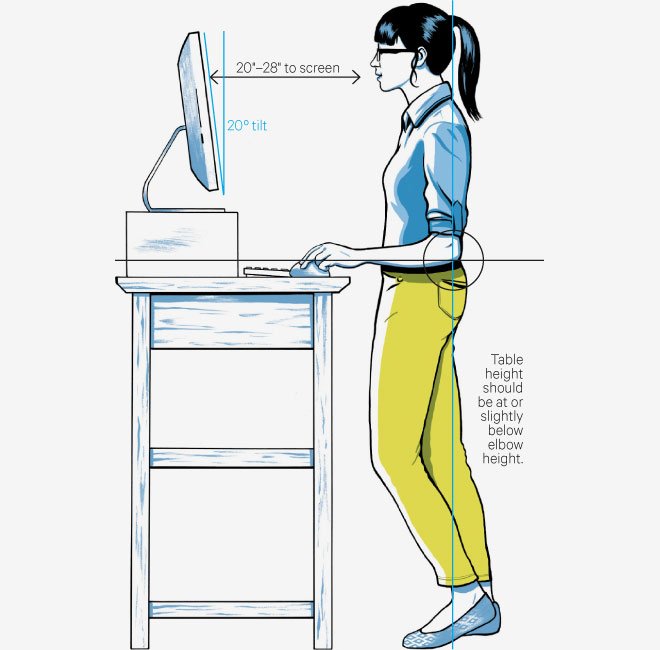 Zami the future of sitting
Zami the future of sittingAnthro
Ergo Standing Desk
HumbleWorks Standing Desk
Sit or Stand Table
Wooden Standing Desk
My Up Desk
Laptop Table
Standup Desk
Floor Stand Tablet PCs
Floor Stand for PCs
A-STAND: Transformable Workstation
Alt-Work Station
Kinesthetic Desks
Stir Kinetic Desk
Lean Chair
Treadmill Desk
Edge Desk
Vari Desk
Sitting to Long
Body Smart
Chiropractic is a form of alternative medicine concerned with the diagnosis and treatment of unverified mechanical disorders of the musculoskeletal system, especially the spine. Proponents believe that such disorders affect general health via the nervous system. The main chiropractic treatment technique involves manual therapy, especially spinal manipulation therapy (SMT), manipulations of other joints and soft tissues. Its foundation is at odds with mainstream medicine, and chiropractic is sustained by pseudoscientific ideas such as subluxation and "innate intelligence".
Inversion Therapy or Inversion Table involves being upside down or at an inverted angle while hanging by the legs, ankles, or feet with the intention of therapeutic benefits. The process of doing so is called inversion. It is a form of spinal decompression and is a form of spinal traction. Gravity boots are ankle supports designed for inversion therapy. Some people use gravity boots to add an extra challenge to workouts, doing inverted crunches or squats. People who have heart disease, high blood pressure, eye diseases (such as glaucoma), or are pregnant are at higher risk for the dangers related to inversion therapy and should consult their doctors about it first. The first time anyone tries inversion therapy with gravity, they should be sure to have someone standing by, in case assistance is required to get out of the apparatus, or if health problems are experienced. During an episode of acid reflux, small amounts of stomach acid may manage to escape from the stomach and into the oesophagus. Typically, gravity minimises this upward leakage but combining an inversion table and acid reflux can be a painful, nauseating, and potentially dangerous combination. Physical Therapy - Pinched Nerve.
Vertebral Column also known as the Backbone or Spine, is part of the axial skeleton. The vertebral column is the defining characteristic of a vertebrate, in which the notochord (a flexible rod of uniform composition) found in all chordates has been replaced by a segmented series of bones—vertebrae separated by intervertebral discs. The vertebral column houses the spinal canal, a cavity that encloses and protects the spinal cord, which is a long, thin, tubular bundle of nervous tissue and support cells that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column. The brain and spinal cord together make up the central nervous system (CNS).
Spinal Cord Injury is damage to the spinal cord that causes changes in its function, either temporary or permanent. These changes translate into loss of muscle function, sensation, or autonomic function in parts of the body served by the spinal cord below the level of the lesion. Injuries can occur at any level of the spinal cord and can be classified as complete injury, a total loss of sensation and muscle function, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord. Depending on the location and severity of damage along the spinal cord, the symptoms can vary widely, from pain or numbness to paralysis to incontinence. The prognosis also ranges widely, from full recovery in rare cases to permanent tetraplegia (also called quadriplegia) in injuries at the level of the neck, and paraplegia in lower injuries. Complications that can occur in the short and long term after injury include muscle atrophy, pressure sores, infections, and respiratory problems. In the majority of cases the damage results from physical trauma such as car accidents, gunshots, falls, or sports injuries, but it can also result from nontraumatic causes such as infection, insufficient blood flow, and tumors. Athletes are especially susceptible to becoming involved in high collision spinal injuries. Some of the more common injuries include any type of sprain and strain of the spinal cord. These injuries can either occur alone, or with another spinal disease. Dislocations and fractures are also common in spine injuries. Efforts to prevent SCI include individual measures such as using safety equipment, societal measures such as safety regulations in sports and traffic, and improvements to equipment. Known since ancient times to be a catastrophic injury and long believed to be untreatable, SCI has seen great improvements in its care since the middle of the 20th century. Treatment of spinal cord injuries starts with stabilizing the spine and controlling inflammation to prevent further damage. Other interventions needed can vary widely depending on the location and extent of the injury, from bed rest to surgery. In many cases, spinal cord injuries require substantial, long-term physical and occupational therapy in rehabilitation, especially if they interfere with activities of daily living. Research into new treatments for spinal cord injuries includes stem cell implantation, engineered materials for tissue support, and wearable robotic exoskeletons. The spine consists of the spinal cord, which is a group of nerves that are protected by the individual vertebrae of the spine. The main function of the spinal cord is to send signals from the brain to other regions of the body. It is the main messenger throughout the body. Myelopathy - Claudication.
Degenerative Disc Disease describes the natural breakdown of an intervertebral disc of the spine. Despite its name, DDD is not considered a disease, nor is it progressively degenerative. On the contrary, disc degeneration is often the effect of natural daily stresses and minor injuries that cause spinal discs to gradually lose water as the anulus fibrosus, or the rigid outer shell of a disc, weakens. As discs weaken and lose water, they begin to collapse. This can result in pressure being put on the nerves in the spinal column, causing pain and weakness. While not always symptomatic, DDD can cause acute or chronic low back or neck pain as well as nerve pain depending on the location of the affected disc and the amount of pressure it places on the surrounding nerve roots. The typical radiographic findings in DDD are black discs, disc space narrowing, vacuum disc, end plate sclerosis, and osteophyte formation. DDD can greatly affect quality of life. Disc degeneration is a disease of micro/macro trauma and of aging, and though for most people is not a problem, in certain individuals a degenerated disc can cause severe chronic pain if left untreated. One third of people aged 40-59 have evidence of degenerative disc disease - Physical Therapy.
Osteoporosis is a disease in which bone weakening increases the risk of a Broken Bone. It is the most common reason for a Broken Bone among the elderly. Bones that commonly break include the vertebrae in the spine, the bones of the forearm, and the hip. Until a broken bone occurs there are typically no symptoms. Bones may weaken to such a degree that a break may occur with minor stress or spontaneously. Chronic pain and a decreased ability to carry out normal activities may occur following a broken bone. Osteoporosis is the leading cause of age-related kyphosis, with sarcopenia, or age-related muscle loss, being a secondary cause. Osteopenia is when your bones are weaker than normal but not so far gone that they break easily, which is the hallmark of osteoporosis.
Kyphosis is a painful condition commonly known as "hunchback" is a physical deformation of the middle and upper spine, in which its natural curve increases, resulting in a "hunched over" posture. Kyphosis is a spinal disorder in which an excessive outward curve of the spine results in an abnormal rounding of the upper back. The condition is sometimes known as "roundback" or—in the case of a severe curve—as "hunchback." Kyphosis can occur at any age, but is common during adolescence. Postural kyphosis (M40.0), the most common type, normally attributed to slouching, can occur in both the old and the young. In the young, it can be called "slouching" and is reversible by correcting muscular imbalances. In the old, it may be a case of hyperkyphosis and called "dowager's hump". There are two different kinds of kyphosis, and they can both affect babies, children, teenagers, and adults. The first type, postural kyphosis, is caused by bad posture and can be corrected by the patient. The second type is caused by a structural disorder and cannot be fixed without medical treatment.
Sarcopenia is the degenerative loss of skeletal muscle mass (0.5–1% loss per year after the age of 50), quality, and strength associated with aging. Sarcopenia is a component of the frailty syndrome. It is often a component of cachexia. It can also exist independently of cachexia; whereas cachexia includes malaise and is secondary to an underlying pathosis (such as cancer), sarcopenia may occur in healthy people and does not necessarily include malaise.
As the Spine and the Muscles that support it become weaker, the vertebrae become susceptible to compression fractures, in which the bone breaks under the load of everyday activities like walking or even coughing. Spinal alignment and curvature can be altered in many ways. They can occur as a result of a birth defect, a child's growth, aging, injury, or previous spine surgery. The most common type of spinal deformity in adults is degenerative scoliosis. Scoliosis is a medical condition in which a person's spine has a sideways curve. The curve is usually "S"- or "C"-shaped over three dimensions. In some, the degree of curve is stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, but severe cases can interfere with breathing. Typically, no pain is present.
Dual-Energy X-Ray Absorptiometry is a means of measuring bone mineral density (BMD). Two X-ray beams, with different energy levels, are aimed at the patient's bones. When soft tissue absorption is subtracted out, the bone mineral density (BMD) can be determined from the absorption of each beam by bone. Dual-energy X-ray absorptiometry is the most widely used and most thoroughly studied bone density measurement technology. The DXA scan is typically used to diagnose and follow osteoporosis, as contrasted to the nuclear bone scan, which is sensitive to certain metabolic diseases of bones in which bones are attempting to heal from infections, fractures, or tumors. (also called DEXA, and quantitative CT, or QCT).
Bone is a rigid organ that constitutes part of the vertebrate skeleton. Bones of the Human Body (image). Bones protect the various organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, and enable mobility. Bones come in a variety of shapes and sizes and have a complex internal and external structure. They are lightweight yet strong and hard, and serve multiple functions. Bone tissue (osseous tissue) is a hard tissue, a type of dense connective tissue. It has a honeycomb-like matrix internally, which helps to give the bone rigidity. Bone tissue is made up of different types of bone cells. Osteoblasts and osteocytes are involved in the formation and mineralization of bone; osteoclasts are involved in the resorption of bone tissue. Modified (flattened) osteoblasts become the lining cells that form a protective layer on the bone surface. The mineralised matrix of bone tissue has an organic component of mainly collagen called ossein and an inorganic component of bone mineral made up of various salts. Bone tissue is a mineralized tissue of two types, cortical bone and cancellous bone. Other types of tissue found in bones include bone marrow, endosteum, periosteum, nerves, blood vessels and cartilage. In the human body at birth, there are over 300 bones, but many of these fuse together during development, leaving a total of 206 separate bones in the adult, not counting numerous small sesamoid bones. The largest bone in the body is the femur or thigh-bone, and the smallest is the stapes in the middle ear. The Greek word for bone is ὀστέον ("osteon"), hence the many terms that use it as a prefix – such as osteopathy. Broken Bones.
Bone Mineral is the inorganic component of bone tissue. It gives bones their compressive strength. Bone mineral is formed from carbonated hydroxyapatite with lower crystallinity. Bone mineral is formed from globular and plate structures distributed among the collagen fibrils of bone and forming yet a larger structure. The bone salt and collagen fibers together constitute the extracellular matrix of bone tissue. Often the plural form "bone salts" is used; it reflects the notion of various salts that, on the level of molecular metabolism, can go into the formation of the hydroxyapatite. Bone mineral is dynamic in living animals; it is continually being resorbed and built anew in the bone remodeling process. In fact, the bones function as a bank or storehouse in which calcium can be continually withdrawn for use or deposited for storage, as dictated by homeostasis, which maintains the concentration of calcium ions in the blood serum within a particular range despite the variability of muscle tissue metabolism. Parathormone and calcitonin are the principal hormones with which the neuroendocrine system controls this ongoing process. The parathyroid and thyroid glands in the neck produce those hormones; thus, problems with those glands (such as hypo- or hyperparathyroidism or hypo- or hyperthyroidism) can create problems with bone mineral density (as well as hypo- or hypercalcemia).
Bone Marrow, the spongy tissue inside most of our bones, produces red blood cells as well as immune cells that help fight off infections and heal injuries. According to a new study of mice and humans, tiny tunnels run from skull bone marrow to the lining of the brain and may provide a direct route for immune cells responding to injuries caused by stroke and other brain disorders.
Strengthen the core and the back. It's important to strengthen the core muscles' ability to stabilize and protect the spine and the back muscles' capability to pull the shoulders and spine into upright posture, resistance-band rows and lat pull-downs, can help strengthen the muscles of the middle and upper back. Supine Y raises (in which you lie on the floor and raise your outstretched arms from the floor to form a Y with your body) and resistance-band pull-aparts, where you hold two ends of a resistance band with your arms in front of your shoulders and pinch your shoulder blades together, focus on the muscles of the upper back. Avoid activities that include spinal flexion or bending and can increase pressure on the vertebra and spinal discs. Protein may help promote strong bones by increasing calcium absorption and affecting hormone levels.
Wolff's law states that bone in a healthy person or animal will adapt to the loads under which it is placed. If loading on a particular bone increases, the bone will remodel itself over time to become stronger to resist that sort of loading. The internal architecture of the trabeculae undergoes adaptive changes, followed by secondary changes to the external cortical portion of the bone, perhaps becoming thicker as a result. The inverse is true as well: if the loading on a bone decreases, the bone will become less dense and weaker due to the lack of the stimulus required for continued remodeling. This reduction in bone density (osteopenia) is known as stress shielding and can occur as a result of a hip replacement (or other prosthesis). The normal stress on a bone is shielded from that bone by being placed on a prosthetic implant.
Massages - The Power of Human Touch
 Massage involves working and acting on
the body with pressure – structured, unstructured, stationary, or moving –
tension, motion, or vibration, done manually or with mechanical aids.
Massage can be applied with the hands, fingers, elbows, knees, forearm,
feet, or a massage device. Depending on the application and technique
used, massage is used to promote
relaxation and well-being, and is
beneficial in treating sports injuries and other problems affecting the
musculature of the body such as postural misalignment and many painful
conditions. In professional settings massage clients are treated while
lying on a massage table, sitting in a massage chair, or lying on a mat on
the floor, while in amateur settings a general purpose surface like a bed
or floor is more common. Aquatic massage and bodywork is performed with
recipients submersed or floating in a warm-water therapy pool.
Massage involves working and acting on
the body with pressure – structured, unstructured, stationary, or moving –
tension, motion, or vibration, done manually or with mechanical aids.
Massage can be applied with the hands, fingers, elbows, knees, forearm,
feet, or a massage device. Depending on the application and technique
used, massage is used to promote
relaxation and well-being, and is
beneficial in treating sports injuries and other problems affecting the
musculature of the body such as postural misalignment and many painful
conditions. In professional settings massage clients are treated while
lying on a massage table, sitting in a massage chair, or lying on a mat on
the floor, while in amateur settings a general purpose surface like a bed
or floor is more common. Aquatic massage and bodywork is performed with
recipients submersed or floating in a warm-water therapy pool.Massage is kneading and rubbing parts of the body to increase circulation and promote relaxation. To manually manipulate someone's body, usually for medicinal or relaxation purposes.
Massage Therapy - Massage Therapy 101 - Massage Therapy - Massage Therapy
Human Touch - Skin (hygiene)
Deep Tissue Rolfing is typically delivered as a series of ten hands-on physical manipulation sessions sometimes called "the recipe". It is based on Rolf's ideas about how the human body's "energy field" can benefit when aligned with the Earth's gravitation field. Practitioners combine superficial and deep manual therapy with movement prompts. The process is sometimes painful.
Deep Tissue Massage is a type of massage that uses forceful strokes to release chronic muscle tension. It targets the deeper layers of muscle and connective tissue. It’s often used to treat muscle damage from injuries. Deep tissue massage is a massage technique that's mainly used to treat musculoskeletal issues, such as strains and sports injuries. It involves applying sustained pressure using slow, deep strokes to target the inner layers of your muscles and connective tissues.
Swedish Massage is a gentle massage technique that will be suitable for you if have a lot of tension or are sensitive to touch. Swedish massage uses long strokes, kneading, and deep circular movements. Vibration and tapping are also used to aid in relaxation. Swedish massage therapy involves soft, long, kneading strokes, as well as light, rhythmic, tapping strokes, on topmost layers of muscles. This is also combined with movement of the joints. By relieving muscle tension, Swedish therapy can be both relaxing and energizing.
Sports Massage is a form of bodywork geared toward participants in athletics. It is used to help prevent injuries, to prepare the body for athletic activity and maintain it in optimal condition, and to help athletes recover from workouts and injuries. Conditions that generally respond well to massage as a complementary therapy include: muscle pain and stiffness, muscle strain, edema or swelling, muscle soreness, muscle sprains, muscle tension, sore spots, repetitive strain injuries and tendinitis. Massage can help these conditions, but it should never be used to replace skilled medical care.
Massage Envy - Myotherapy
Erotic Massage is the use of massage techniques by a person on another person's erogenous zones to achieve or enhance their sexual excitation or arousal and to achieve orgasm. Massages have been used for medical purposes for a very long time, and their use for erotic purposes also has a long history. In the case of women, the two focal areas are the breasts and pubis, while in case of men, the focal area is the male genitals. When the massage is of a partner's genitals, the act is usually referred to as mutual masturbation. Today, erotic massage is used by some people on occasion as a part of sex, either as foreplay or as the final sex act, or as part of sex therapy. There is also a large commercial erotic massage industry in some countries and cities.
Muscle Knots - Trigger Points
Trigger Point is a sensitive area in the muscle or connective tissue or fascia that becomes painful when compressed. Pressing on a trigger point can cause referred pain and can help identify the external area in the body generating the pain.
Muscle Knots are hard, sensitive areas of muscles that tighten and contract even when the muscle is at rest. These tense muscle fibers can cause pain in other parts of the body when touched. They’re also known as trigger points. Muscle knots can be caused by a sedentary lifestyle, overusing or injuring your muscles or poor posture. Other factors include dehydration, unhealthy eating habits, and stress and anxiety may also contribute to muscle knots. Muscle knots can occur anywhere in the body, but they’re usually found in your back, shoulders, and neck. They often show up in your gluteal muscles, too. Muscles knots can cause aching sensations and pain in your muscles and joints. When you touch a muscle knot, it may feel swollen, tense, or bumpy. It could also feel tight and contracted, even when you’re trying to relax, and they’re often sensitive to the touch. The affected area may even become inflamed or swollen. Muscle knots can cause symptoms in areas outside of the muscles, including: headaches, toothaches and earaches. You may also experience stress, anxiety, and depression, and have difficulty sleeping. Untreated muscle knots can cause chronic pain and lead to other health issues. See your health care provider if you’ve taken measures to relieve your muscle pain, but it persists. You should also call your doctor if pain becomes severe and is interfering with your daily life and well-being. It’s possible that what seems like a muscle knot could be something else, such as a swollen lymph node. Usually there will be other symptoms that accompany a swollen lymph node, such as a cold, cough, or infection. Check with a doctor, physical therapist, or osteopath if you want to make sure it’s a muscle knot and not something else. They can determine possible causes for the pain. Self-Massage in some cases can help to relieve the sore muscles yourself. Locate the muscle knot and use your fingers to gently massage it. While massaging, focus on trying to loosen up the tight muscle fibers and relieve tension. Press firmly into the affected area and make small circles with your fingers. You can also place a tennis ball between your back and the floor or a wall, and roll back and forth on the ball to apply more pressure to the knot. Experiment by slowly and gently moving the ball to apply pressure to points of tension. You can use a foam roller in much the same way. To get rid of the knots, you’ll need to break up the knotted tissue and calm inflamed nerves. You can use massage to treat muscle knots. Massage therapy increases circulation and improves blood flow. That can improve muscle function and help loosen up your muscles. This helps to relieve pain and stiffness. Keep in mind that one session isn’t usually enough to heal you completely. You’ll likely need to have several frequent sessions. Once you see improvements you can space out your sessions. There are several types of massage. The type you’ll benefit from most will depend on the severity of your muscle knots and your personal preference. You may need to try several different types of massage before you find a type that you like. Put pressure on the muscle knot until it softens and releases. After a treatment session, you’ll have a set of movements to complete at home. This will help to retrain your muscles. A physical therapist can help you identify the underlying causes of your muscle knots. They will treat your pain using treatments appropriate to your case. You will be taught techniques that will reduce pain and prevent it from recurring. Gentle stretching that elongates your muscles can help you to release tension in your body. Aerobic exercise may help to relieve muscle knots. Muscle rubs help to soften and relax muscle knots. You can massage a muscle rub onto the affected area twice a day for cooling relief. You may need someone to help you apply to it difficult-to-reach areas. Using a combination of heat and cold can help to relieve pain and inflammation due to muscle knots. Cold helps to constrict the blood vessel, which reduces swelling. To apply cold, use a cold compress for 10 minutes, and then remove it for at least 15 minutes. You can repeat this until you begin to find relief. Heat relaxes and loosens stiff muscles, and relieves pain. Heat may increase blood flow, which promotes healing. To apply heat, use a heating pad or take a warm bath. Alternate between cold and heat treatment, or use the one that works best for you. Hot and cold therapy should be used in conjunction with other therapies. Prevention - There are several ways to prevent muscle knots from forming. Always practice good posture in your daily life. Focus on sitting relaxed, with your shoulders back and down, and avoid slouching while sitting. Get plenty of rest and adequate exercise. Warm up and cool down when exercising, and don’t overexert yourself. Lifting too heavy or running too fast can cause injuries that may also lead to muscle knots. Don’t sit for long periods of time. Take a break, and get up and move at least once every hour of extended sitting. Do simple stretches throughout the day to keep your muscles from getting tight. You can even do exercises while sitting at a desk or watching television. Bring an awareness of the alignment of your body while going about physical activities. Maintain a healthy diet that includes calcium, potassium, and magnesium, and drink plenty of water. Replace processed foods with fresh, whole foods. Consider getting regular massages to help you to relax, gain flexibility, and keep your muscles healthy.
Metamorphic Technique is an Alternative Medicine involving application of pressure to the feet and hands with specific thumb, finger, and hand techniques without the use of oil or lotion. It is based on a system of zones and reflex areas that purportedly reflect an image of the body on the feet and hands, with the premise that such work effects a physical change to the body.
Body Mechanics (youtube) - Message Video (youtube) - Message (youtube)
Stiff Neck Message (youtube) - Massage Therapy (netflix)
Osteopathy is a type of alternative medicine that emphasizes massage and other physical manipulation of muscle tissue and bones. "sensitive to" or "responding to".
U-GYM Mini: Digital Muscle Stimulator
Acupressure is an alternative medicine technique similar in principle to acupuncture. It is based on the concept of life energy which flows through "meridians" in the body. In treatment, physical pressure is applied to acupuncture points with the aim of clearing blockages in these meridians. Pressure may be applied by hand, by elbow, or with various devices. Some medical studies have suggested that acupressure may be effective at helping manage nausea and vomiting, for helping lower back pain, tension headaches, stomach ache, among other things, although such studies have been found to have a high likelihood of bias. Like many alternative medicines, it may benefit from a placebo effect.
Acupressure - Acupressure Institute - Human Touch
Acupressure Online - YouTube Acupressure Video
Reflexology is an alternative medicine involving application of pressure to the feet and hands with specific thumb, finger, and hand techniques without the use of oil or lotion. It is based on a system of zones and reflex areas that purportedly reflect an image of the body on the feet and hands, with the premise that such work effects a physical change to the body. Always pay attention to any unusual changes. Don't over do it. Academy of Reflexology - Reflexology.
Hand Reflexology (image of areas) - Foot Reflexology (image chart) - Face Message Points (image of areas)
Acupuncture is a form of Alternative Medicine in which thin needles are inserted into the body. It is a key component of traditional Chinese medicine (TCM). TCM theory and practice are not based upon scientific knowledge, and acupuncture is a pseudoscience. There are a diverse range of acupuncture theories based on different philosophies, and techniques vary depending on the country. The method used in TCM is likely the most widespread in the US. It is most often used for pain relief, though it is also used for a wide range of other conditions. Acupuncture is generally used only in combination with other forms of treatment. If you do acupuncture correctly, your body releases more nitric oxide at the points where the needles are inserted. The nitric oxide increases blood flow and triggers your body to release natural anesthetics.
Electroacupuncture According to Voll is a form of acupuncture where a small electric current is passed between pairs of acupuncture needles. According to some acupuncturists[who?], this practice augments the use of regular acupuncture, can restore health and well-being, and is particularly good for treating pain[citation needed]. There is evidence for some efficacy (when used in addition to antiemetics) in treating moderate post-chemotherapy vomiting, but not for acute vomiting or delayed nausea severity.
More than Four Hundred Acupuncture Points have been described, with the majority located on one of the main meridians, pathways which run throughout the body and according to Traditional Chinese Medicine (TCM) transport life energy (qi, 氣).
Acupuncture - Oriental Chinese Medicine - Medical Acupuncture
Nitric Oxide is a molecular, chemical compound with chemical formula of ·NO with a short half-life of a few seconds in the blood. Nitric oxide is a free radical. Nitric oxide is an important cellular signaling molecule involved in many physiological and pathological processes. It is a powerful vasodilator which results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins (called venodilators), large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, which is the narrowing of blood vessels.
Meridian is a concept in traditional Chinese medicine (TCM) about a path through which the life-energy known as "qi" flows.
Meridians (youtube) - Meridian Tapping Techniques - MTT
Meridian Tapping Technique (youtube) - Meridian Tapping (youtube)
Instantly Double Your Lung Oxygen Level (Created by Dr Alan Mandell, DC) (youtube) - Squeeze thumb tip - Press on thumb base for 1 minute - Parasympathetic Nervous System.
Chakras - Soothing Sounds - Jumping Benefits
Emotional Freedom Technique is a form of counseling intervention that draws on various theories of alternative medicine including acupuncture, neuro-linguistic programming, energy medicine, and Thought Field Therapy or TFT. It is best known through Gary Craig's EFT Handbook, published in the late 1990s, and related books and workshops by a variety of teachers. EFT and similar techniques are often discussed under the umbrella term "energy psychology". Placebos.
Facial Massage - Saving Face
 Facial Toning
is a type of cosmetic procedure or physical therapy tool which promises to
alter facial contours by means of increasing muscle tone, and facial
volume by promoting muscular hypertrophy, and preventing muscle loss due
to aging or facial paralysis. Facial toning and exercise is therefore in
part a technique to achieve facial rejuvenation by reducing wrinkles,
sagging and expression marks on the face and
skin. As a physical therapy,
facial toning is used for victims of stroke and forms of facial paralysis
such as Bell’s palsy. Facial toning achieves this by performing facial
muscle exercising. There are two types of facial toning exercises: active
and passive face exercises. Body Message.
Facial Toning
is a type of cosmetic procedure or physical therapy tool which promises to
alter facial contours by means of increasing muscle tone, and facial
volume by promoting muscular hypertrophy, and preventing muscle loss due
to aging or facial paralysis. Facial toning and exercise is therefore in
part a technique to achieve facial rejuvenation by reducing wrinkles,
sagging and expression marks on the face and
skin. As a physical therapy,
facial toning is used for victims of stroke and forms of facial paralysis
such as Bell’s palsy. Facial toning achieves this by performing facial
muscle exercising. There are two types of facial toning exercises: active
and passive face exercises. Body Message.Facial Massage (youtube)
Facial Massage: Face Lift 2:30 (youtube)
Facial Yoga and Meditation 10 (youtube)
Face Yoga (youtube)
Happy Face Yoga Facial Exercises For a Younger Face.
Facial and Shoulder Massage (youtube)
Tanaka Face (youtube)
Self Massage (youtube)
Lymph Massage Techniques (youtube)
Lymph Drainage Massage (youtube)
Facial is a family of skin care treatments for the face, including steam, exfoliation, extraction, creams, lotions, facial masks, peels, and massage. They are normally performed in beauty salons, but are also a common spa treatment. They are used for general skin health as well as for specific skin conditions. Types of facials include European facial, LED light therapy facials, hydrafacials and mini-facials.
Save Face is to preserve one's dignity and avoid having other people lose respect for you. To retain respect and avoid humiliation. Not Being a Sell Out.
Face is sociological concept and a class of behaviors and customs operating (active) in different countries and cultures, associated with the morality, honor, and authority of an individual (or group of individuals), and its image in social groups.
Bathing (hygiene) - Increase-Blood-Flow - Improve-Blood-Circulation
Cranial Nerves are the nerves that emerge directly from the brain, including the brainstem, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing. The cranial nerves emerge from the central nervous system above the level of the first vertebrae of the vertebral column. Each cranial nerve is paired and is present on both sides. There are conventionally twelve pairs of cranial nerves, which are described with Roman numerals I–XII. Some considered there to be thirteen pairs of cranial nerves, including cranial nerve zero. The numbering of the cranial nerves is based on the order in which they emerge from the brain and brainstem, from front to back. The terminal nerves (0), olfactory nerves (I) and optic nerves (II) emerge from the cerebrum, and the remaining ten pairs arise from the brainstem, which is the lower part of the brain. The cranial nerves are considered components of the peripheral nervous system (PNS), although on a structural level the olfactory (I), optic (II), and trigeminal (V) nerves are more accurately considered part of the central nervous system (CNS). The cranial nerves are in contrast to spinal nerves, which emerge from segments of the spinal cord.
Olfactory Nerve contains sensory nerve fibers relating to the sense of smell. the olfactory nerve is somewhat unusual among cranial nerves because it is capable of some regeneration if damaged. The olfactory nerve is sensory in nature and originates on the olfactory mucosa in the upper part of the nasal cavity. From the olfactory mucosa, the nerve (actually many small nerve fascicles) travels up through the cribriform plate of the ethmoid bone to reach the surface of the brain. Here the fascicles enter the olfactory bulb and synapse there; from the bulbs (one on each side) the olfactory information is transmitted into the brain via the olfactory tract. The fascicles of the olfactory nerve are not visible on a cadaver brain because they are severed upon removal. The olfactory nerve transmits sensory information to your brain regarding smells that you encounter.
Optic Nerve is a paired cranial nerve that transmits visual information from the retina to the brain. In humans, the optic nerve is derived from optic stalks during the seventh week of development and is composed of retinal ganglion cell axons and glial cells; it extends from the optic disc to the optic chiasma and continues as the optic tract to the lateral geniculate nucleus, pretectal nuclei, and superior colliculus.
Oculomotor Nerve are the eye muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation (ability to focus on near objects as in reading). The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement. The oculomotor nerve has two different motor functions: muscle function and pupil response. Muscle function. Your oculomotor nerve provides motor function to four of the six muscles around your eyes. These muscles help your eyes move and focus on objects. Pupil response. It also helps to control the size of your pupil as it responds to light. When light enters your eye, it comes into contact with special receptors in your retina called rods and cones. Rods are found in large numbers and are highly sensitive to light. They’re more specialized for black and white or night vision. Cones are present in smaller numbers. They have a lower light sensitivity than rods and are more involved with color vision. The information received by your rods and cones is transmitted from your retina to your optic nerve. Once inside your skull, both of your optic nerves meet to form something called the optic chiasm. At the optic chiasm, nerve fibers from half of each retina form two separate optic tracts. Through each optic tract, the nerve impulses eventually reach your visual cortex, which then processes the information. Your visual cortex is located in the back part of your brain.
Trochlear Nerve is your superior oblique muscle. This is the muscle that’s responsible for downward, outward, and inward eye movements.
Abducens Nerve controls the movement of the lateral rectus muscle, responsible for outward gaze. It is a somatic efferent nerve. This muscle is involved in outward eye movement. For example, you would use it to look to the side.
Trigeminal Nerve is the largest of your cranial nerves and has both sensory and motor functions. The trigeminal nerve has three divisions, which are the ophthalmic division, which sends sensory information from the upper part of your face, including your forehead, scalp, and upper eyelids. The maxillary division communicates sensory information from the middle part of your face, including your cheeks, upper lip, and nasal cavity. The mandibular division has both a sensory and a motor function. It sends sensory information from your ears, lower lip, and chin. It also controls the movement of muscles within your jaw and ear.
Facial Nerve emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. The nerves typically travels from the pons through the facial canal in the temporal bone and exits the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI (abducens nerve) and anterior to cranial nerve VIII (vestibulocochlear nerve). The facial nerve also supplies preganglionic parasympathetic fibers to several head and neck ganglia. The facial and intermediate nerves can be collectively referred to as the nervus intermediofacialis. Facial nerve provides both sensory and motor functions, including: moving muscles used for facial expressions as well as some muscles in your jaw providing a sense of taste for most of your tongue, supplying glands in your head or neck area, such as salivary glands and tear-producing glands, communicating sensations from the outer parts of your ear. Your facial nerve has a very complex path. It originates in the pons area of your brainstem, where it has both a motor and sensory root. Eventually, the two nerves fuse together to form the facial nerve. Both within and outside of your skull, the facial nerve branches further into smaller nerve fibers that stimulate muscles and glands or provide sensory information. Face Message Points (image of areas)
Vestibulocochlear Nerve transmits sound and equilibrium (balance) information from the inner ear to the brain. Through olivocochlear fibers, it also transmits motor and modulatory information from the superior olivary complex in the brainstem to the cochlea. known as the eighth cranial nerve, vestibulocochlear nerve has sensory functions involving hearing and balance. It consists of two parts, the cochlear portion and vestibular portion: Cochlear portion. Specialized cells within your ear detect vibrations from sound based off of the sound’s loudness and pitch. This generates nerve impulses that are transmitted to the cochlear nerve. Vestibular portion. Another set of special cells in this portion can track both linear and rotational movements of your head. This information is transmitted to the vestibular nerve and used to adjust your balance and equilibrium. The cochlear and vestibular portions of your vestibulocochlear nerve originate in separate areas of the brain. The cochlear portion starts in an area of your brain called the inferior cerebellar peduncle. The vestibular portion begins in your pons and medulla. Both portions combine to form the vestibulocochlear nerve.
Glossopharyngeal Nerve is a mixed nerve that carries afferent sensory and efferent motor information. It exits the brainstem out from the sides of the upper medulla, just anterior (closer to the nose) to the vagus nerve. The motor division of the glossopharyngeal nerve is derived from the basal plate of the embryonic medulla oblongata, while the sensory division originates from the cranial neural crest. Glossopharyngeal nerve has both motor and sensory functions, including: sending sensory information from your sinuses, the back of your throat, parts of your inner ear, and the back part of your tongue, providing a sense of taste for the back part of your tongue, stimulating voluntary movement of a muscle in the back of your throat called the stylopharyngeus. The glossopharyngeal nerve originates in a part of your brainstem called the medulla oblongata. It eventually extends into your neck and throat region.
Vagus Nerve interfaces with the parasympathetic control of the heart, lungs, and digestive tract. The vagus nerves are normally referred to in the singular. It is the longest nerve of the autonomic nervous system in the human body and comprises sensory and motor fibers. The sensory fibers originate from neurons of the nodose ganglion, whereas the motor fibers come from neurons of the dorsal motor nucleus of the vagus and the nucleus ambiguus. Vagus nerve is a very diverse nerve. It has both sensory and motor functions, including: communicating sensation information from your ear canal and parts of your throat, sending sensory information from organs in your chest and trunk, such as your heart and intestines, allowing motor control of muscles in your throat, stimulating the muscles of organs in your chest and trunk, including those that move food through your digestive tract (peristalsis), providing a sense of taste near the root of your tongue. Out of all of the cranial nerves, the vagus nerve has the longest pathway. It extends from your head all the way into your abdomen. It originates in the part of your brainstem called the medulla.
Accessory Nerve is a cranial nerve that supplies the sternocleidomastoid and trapezius muscles. It is considered as the eleventh of twelve pairs of cranial nerves, or simply cranial nerve XI, as part of it was formerly believed to originate in the brain. The sternocleidomastoid muscle tilts and rotates the head, while the trapezius muscle, connecting to the scapula, acts to shrug the shoulder. Traditional descriptions of the accessory nerve divide it into a spinal part and a cranial part. The cranial component rapidly joins the vagus nerve, and there is ongoing debate about whether the cranial part should be considered part of the accessory nerve proper. Consequently, the term "accessory nerve" usually refers only to nerve supplying the sternocleidomastoid and trapezius muscles, also called the spinal accessory nerve. Strength testing of these muscles can be measured during a neurological examination to assess function of the spinal accessory nerve. Poor strength or limited movement are suggestive of damage, which can result from a variety of causes. Injury to the spinal accessory nerve is most commonly caused by medical procedures that involve the head and neck. Injury can cause wasting of the shoulder muscles, winging of the scapula, and weakness of shoulder abduction and external rotation. The accessory nerve is derived from the basal plate of the embryonic spinal segments C1–C6. Accessory nerve is a motor nerve that controls the muscles in your neck. These muscles allow you to rotate, flex, and extend your neck and shoulders. It’s divided into two parts: spinal and cranial. The spinal portion originates in the upper part of your spinal cord. The cranial part starts in your medulla oblongata. These parts meet briefly before the spinal part of the nerve moves to supply the muscles of your neck while the cranial part follows the vagus nerve.
Hypoglossal Nerve is the twelfth cranial nerve, hypoglossal nerve is the 12th cranial nerve which is responsible for the movement of most of the muscles in your tongue. It starts in the medulla oblongata and moves down into the jaw, where it reaches the tongue. Hypoglossal nerve innervates all the extrinsic and intrinsic muscles of the tongue, except for the palatoglossus which is innervated by the vagus nerve. It is a nerve with a solely motor function. The nerve arises from the hypoglossal nucleus in the medulla as a number of small rootlets, passes through the hypoglossal canal and down through the neck, and eventually passes up again over the tongue muscles it supplies into the tongue. The nerve is involved in controlling tongue movements required for speech and swallowing, including sticking out the tongue and moving it from side to side. Damage to the nerve or the neural pathways which control it can affect the ability of the tongue to move and its appearance, with the most common sources of damage being injury from trauma or surgery, and motor neuron disease. The first recorded description of the nerve is by Herophilos in the third century BC. The name hypoglossus springs from the fact that its passage is below the tongue, from hypo (Greek: "under") and glossa (Greek: "tongue").
Head is the part of an organism which usually includes the ears, brain, forehead, cheeks, chin, eyes, nose, and mouth, each of which aid in various sensory functions such as sight, hearing, smell, and taste, respectively. Some very simple animals may not have a head, but many bilaterally symmetric forms do, regardless of size. Heads develop in animals by an evolutionary trend known as cephalization. In bilaterally symmetrical animals, nervous tissues concentrate at the anterior region, forming structures responsible for information processing. Through biological evolution, sense organs and feeding structures also concentrate into the anterior region; these collectively form the head.
Human Skull is the bony structure that forms the head in the human skeleton. It supports the structures of the face and forms a cavity for the brain. Like the skulls of other vertebrates, it protects the brain from injury. The skull consists of three parts, of different embryological origin—the neurocranium, the sutures, and the facial skeleton (also called the membraneous viscerocranium). The neurocranium (or braincase) forms the protective cranial cavity that surrounds and houses the brain and brainstem. The upper areas of the cranial bones form the calvaria (skullcap). The membranous viscerocranium includes the mandible. The sutures are fairly rigid joints between bones of the neurocranium. The facial skeleton is formed by the bones supporting the face.
Occipital Bun is a prominent bulge or projection of the occipital bone at the back of the skull. While common among many of humankind's ancestors, primarily robust relatives rather than gracile, the protrusion is still relatively prevalent in modern Homo sapiens. It is suspected that occipital buns might correlate with the biomechanics of running. Another as yet unsubstantiated theory attributes them to enlargement of the cerebellum, a region of the brain which mediates the timing of motor actions and spatial reasoning. There are still some human populations which often exhibit occipital buns. A greater proportion of early modern Europeans had them, but extremely prominent occipital buns in modern populations are now fairly infrequent. A study conducted by Lieberman, Pearson and Mowbray provides evidence that individuals with narrow heads (dolichocephalic) or narrow cranial bases and relatively large brains are more likely to have occipital buns as a means of resolving a spatial packing problem. Occipital Bun is also called occipital spurs, occipital knob, chignon hooks or inion hooks.
Occipital Bone is a cranial dermal bone and the main bone of the occiput on the back and lower part of the skull. It is trapezoidal in shape and curved on itself like a shallow dish. The occipital bone overlies the occipital lobes of the cerebrum. At the base of skull in the occipital bone, there is a large oval opening called the foramen magnum, which allows the passage of the spinal cord. Like the other cranial bones, it is classed as a flat bone. Due to its many attachments and features, the occipital bone is described in terms of separate parts. From its front to the back is the basilar part, also called the basioccipital, at the sides of the foramen magnum are the lateral parts, also called the exoccipitals, and the back is named as the squamous part. The basilar part is a thick, somewhat quadrilateral piece in front of the foramen magnum and directed towards the pharynx. The squamous part is the curved, expanded plate behind the foramen magnum and is the largest part of the occipital bone. Due to its embryonic derivation from paraxial mesoderm (as opposed to neural crest, from which many other craniofacial bones are derived), it has been posited that "the occipital bone as a whole could be considered as a giant vertebra enlarged to support the brain."
Doctors - Resources
Compare Doctors
Compare Doctors
Doc Info
Surgeon Ratings
Rate MD's
Provider Search
Healthcare Quality Research
Healthcare Quality
Consumer Lab
Healthy Stuff
Small Step
Energy Times
HealthCare Ratings
Patient Opinion
Doctor Ratings Reviews
Quack Watch
Physicians Social Network
Doctor Base
Medical Error's
Compare Hospitals
Hospital Compare
Compare Hospitals Healthcare
Doctors & Hospitals Reviews
Quality Net
High Value Care
Science & Health Information
Clinicians
Product Consumer Safety
Wait Times
E. R. Wait Times
Emergency Department
E.R. Visits
E.D. Overuse (pdf)
Unnecessary Tests Procedures
Hospital Emergency Codes (wiki)
Medical Classification
Acute Care
Chronic
Wounds
Respiratory Infections
Abdominal Pains
Compare Doctors
Doc Info
Surgeon Ratings
Rate MD's
Provider Search
Healthcare Quality Research
Healthcare Quality
Consumer Lab
Healthy Stuff
Small Step
Energy Times
HealthCare Ratings
Patient Opinion
Doctor Ratings Reviews
Quack Watch
Physicians Social Network
Doctor Base
Medical Error's
Compare Hospitals
Hospital Compare
Compare Hospitals Healthcare
Doctors & Hospitals Reviews
Quality Net
High Value Care
Science & Health Information
Clinicians
Product Consumer Safety
Wait Times
E. R. Wait Times
Emergency Department
E.R. Visits
E.D. Overuse (pdf)
Unnecessary Tests Procedures
Hospital Emergency Codes (wiki)
Medical Classification
Acute Care
Chronic
Wounds
Respiratory Infections
Abdominal Pains
Medical Error's
Examinations
Patient Safety
Patient Safety
Patient Safety Network
Safe Patient Project
Questions to Ask
Patient Safety Foundation
Patient Safety
Patient Safety Focus
Safer Patients
Joint Commission
Superbug Antibiotic Resistance
Klebsiella Pneumoniae
Quality Safety
Drug Dangers
Check Lists
Ct Center for Patient Safety
Health Policies
Public Health Agencies
Heath Care Improvement
Health Care Reform
Elderly Care
Disabled Care
Brain - Memory
People Smart
Information Resources
Human Sexuality
Child Birth
Our Medical Data Must Become Free Data generated by your body is routinely captured and sold by healthcare companies. Shouldn’t you benefit from it, too?
Federally-Funded Health Centers
Access to Quality Health Care.
Examinations
Patient Safety
Patient Safety
Patient Safety Network
Safe Patient Project
Questions to Ask
Patient Safety Foundation
Patient Safety
Patient Safety Focus
Safer Patients
Joint Commission
Superbug Antibiotic Resistance
Klebsiella Pneumoniae
Quality Safety
Drug Dangers
Check Lists
Ct Center for Patient Safety
Health Policies
Public Health Agencies
Heath Care Improvement
Health Care Reform
Elderly Care
Disabled Care
Brain - Memory
People Smart
Information Resources
Human Sexuality
Child Birth
Our Medical Data Must Become Free Data generated by your body is routinely captured and sold by healthcare companies. Shouldn’t you benefit from it, too?
Federally-Funded Health Centers
Access to Quality Health Care.
Antibiotics
Vaccines
Travel Health Advice
Disease Outbreaks
Allergies - Germs
Wash your Hands
Hospital Infections
Colds - Flu
Pulse Oximetry
Vital Signs
Medical Ultrasonography
Automated External Defibrillator
AED Locator
Locate
Science Websites
CPR
Cardiopulmonary Resuscitation
Membrane Oxygenation
Privacy
Privacy
Physician Patient Privilege
Confidentiality
Non-Disclosure Agreement
Release Form
Doctors Oath
We Consent Donate Data
Data Protection
HIPAA
Health Insurance Portability
and Accountability Act
Department of Health &
Human Services
Methodology: How We
Analyzed Privacy Violation Data
Vaccines
Travel Health Advice
Disease Outbreaks
Allergies - Germs
Wash your Hands
Hospital Infections
Colds - Flu
Pulse Oximetry
Vital Signs
Medical Ultrasonography
Automated External Defibrillator
AED Locator
Locate
Science Websites
CPR
Cardiopulmonary Resuscitation
Membrane Oxygenation
Privacy
Privacy
Physician Patient Privilege
Confidentiality
Non-Disclosure Agreement
Release Form
Doctors Oath
We Consent Donate Data
Data Protection
HIPAA
Health Insurance Portability
and Accountability Act
Department of Health &
Human Services
Methodology: How We
Analyzed Privacy Violation Data
Health Records
Personal Health Records
Online Medical Records
Electronic Health Record
Medical Information Online
Online Personal Health Record
Personal Health Record
Health Systems
Google Health
Patients Like Me
Everyday Health
Life Goes Strong
Spark People
Revolution Health
Heathcare IT
Epic
American Telemed
Health Information Exchange
Project baseline quest to collect comprehensive health data and use it as a map and compass, pointing the way to disease prevention.
Pharmaceutical Dangers
Mental Health Websites
IHME Institute for Health
Metrics and Evaluation
Medical Scribe (wiki)
I am Scribe
Women and Medications
Medications Information
Documentaries
Medical Questions Farming Info
Water Safety
Free Medical Clinics
Broken Bones
Info
Personal Health Records
Online Medical Records
Electronic Health Record
Medical Information Online
Online Personal Health Record
Personal Health Record
Health Systems
Google Health
Patients Like Me
Everyday Health
Life Goes Strong
Spark People
Revolution Health
Heathcare IT
Epic
American Telemed
Health Information Exchange
Project baseline quest to collect comprehensive health data and use it as a map and compass, pointing the way to disease prevention.
Pharmaceutical Dangers
Mental Health Websites
IHME Institute for Health
Metrics and Evaluation
Medical Scribe (wiki)
I am Scribe
Women and Medications
Medications Information
Documentaries
Medical Questions Farming Info
Water Safety
Free Medical Clinics
Broken Bones
Info
Health News - Health Resources
Health News
Health News
Health Statistics by State
Medical News Today
Food History News
Med Page Today
My Health News Daily
Kaiser Health News
The Community Guide
Medical Xpress
Academy of Family Physicians
Biomed Research Articles
Natural News
Coding News in Health Care
Reporting on Health
Health Key
Nurse Anesthetists
Global Health and Poverty
National Health Federation
National Health Freedom
Institute of Medicine
Stat News
EMS World Magazine
Global Health Now forum for news and information for the global health community.
Dmoz Health Websites
Women's News
Health, Mind & Body Books
Multilingual Health Information
Health in Spanish
Vaccines
Health News
Health Statistics by State
Medical News Today
Food History News
Med Page Today
My Health News Daily
Kaiser Health News
The Community Guide
Medical Xpress
Academy of Family Physicians
Biomed Research Articles
Natural News
Coding News in Health Care
Reporting on Health
Health Key
Nurse Anesthetists
Global Health and Poverty
National Health Federation
National Health Freedom
Institute of Medicine
Stat News
EMS World Magazine
Global Health Now forum for news and information for the global health community.
Dmoz Health Websites
Women's News
Health, Mind & Body Books
Multilingual Health Information
Health in Spanish
Vaccines
Health Questions
Web MD
E-Medicine
E-Medicine Health
Medpedia
Doctor Base
Organized Wisdom
Personalized Medicine
Medicine Net
Clinical Community
Keas
Prevention
Kid Netic
Health Finder
Health Central
Health Line
Healthy
Quality Health
Healthopedia
Real Age
Well Sphere
American Pediatrics
American Collage of Physicians
Plane Tree
Pediatric Education
E Health Forum
Share Care
Med Help
Wrong Diagnosis
Right Health
Medicine Online
Family Doctor
Health Grades
Academy Medical Education
Medical Questions
MD Consult
Health Tap
Inpatient or Outpatient (PDF)
E Health Forum
Health Questions
Q&A Websites
Real Self
What Effects my Health (PDF)
Web MD
E-Medicine
E-Medicine Health
Medpedia
Doctor Base
Organized Wisdom
Personalized Medicine
Medicine Net
Clinical Community
Keas
Prevention
Kid Netic
Health Finder
Health Central
Health Line
Healthy
Quality Health
Healthopedia
Real Age
Well Sphere
American Pediatrics
American Collage of Physicians
Plane Tree
Pediatric Education
E Health Forum
Share Care
Med Help
Wrong Diagnosis
Right Health
Medicine Online
Family Doctor
Health Grades
Academy Medical Education
Medical Questions
MD Consult
Health Tap
Inpatient or Outpatient (PDF)
E Health Forum
Health Questions
Q&A Websites
Real Self
What Effects my Health (PDF)
Publications
Library of Medicine
PubMed 20 Million Citations
Network Libraries of Medicine
Future of Medicine
Pediatrics Publications
Plos Medicine
Annals of Internal Medicine
Research Sources
Journal of Medical
Internet Research
Clinical Research with
Real Life Experience
British Medical Journal
N. E. Journal of Medicine
Biomedical Search
Jama Network
Kaiser Family Foundation
Rosalynn Cater Care Giving
Care Coordination Programs
The Permanente Journal
a peer-reviewed journal of medical science, social science in medicine, and medical humanities.
Medline Plus.gov
Research Flaws
Health Surveys
Global School-Based Student Health Survey
The World Health Survey
Nat. Health Interview Survey
Demographic Health Surveys
Center for Health Statistics
Question Pro
Ratings
Public Surveys
Library of Medicine
PubMed 20 Million Citations
Network Libraries of Medicine
Future of Medicine
Pediatrics Publications
Plos Medicine
Annals of Internal Medicine
Research Sources
Journal of Medical
Internet Research
Clinical Research with
Real Life Experience
British Medical Journal
N. E. Journal of Medicine
Biomedical Search
Jama Network
Kaiser Family Foundation
Rosalynn Cater Care Giving
Care Coordination Programs
The Permanente Journal
a peer-reviewed journal of medical science, social science in medicine, and medical humanities.
Medline Plus.gov
Research Flaws
Health Surveys
Global School-Based Student Health Survey
The World Health Survey
Nat. Health Interview Survey
Demographic Health Surveys
Center for Health Statistics
Question Pro
Ratings
Public Surveys
Health.gov
Health Care.gov
US Department of Health
Surgeon General
Health
American Medical Association
Cleveland Clinic
Mayo Clinic
John Hopkins
Aids
Avert
Data
Viruses
Procaare
APOBEC3G
Immune Therapy
Parkinson's Voice
Medicare 800.633.4227
Medicare Advocacy
CS Mott Children's Hospital: University of Michigan Health System
University of Michigan Health System
Diseases
Health Care.gov
US Department of Health
Surgeon General
Health
American Medical Association
Cleveland Clinic
Mayo Clinic
John Hopkins
Aids
Avert
Data
Viruses
Procaare
APOBEC3G
Immune Therapy
Parkinson's Voice
Medicare 800.633.4227
Medicare Advocacy
CS Mott Children's Hospital: University of Michigan Health System
University of Michigan Health System
Diseases
Always Ask Questions - Medical Errors
When seeking help always get a second or third opinion from a professional source or a very intelligent well trusted friend or family member. There's a lot of fraud, false medical claims and Doctors over prescribing medications. So please do your homework, especially with medications and treatment alternatives. Compliance is only expectable after you have done your Research. Don't just consult a physician, you need to ask several experts who have varying degrees of knowledge.
Is surgery necessary? Is medication necessary? What are my options? What are the risks? What happens if I do nothing?
Be positive and be hopeful but don't be Gullible. Not all Doctors are Honest or Educated, so it's not just about who you can trust. Remember that experts make mistakes too. 4 out of 10 doctors Misdiagnose their patients. There's also Over Diagnosis and underdiagnosed. And please don't worry. Ask questions and learn as much as you can. Some Doctors are like car mechanics, they don't want to show you how to do your own maintenance, because then they would get less business from you and make less money. They want you to come back for a reason, and it's not because they like you. We can't provide effective, efficient, healthy, logical and fair services when people are driven by greed. We need to improve. We can't encourage people to be selfish and egotistical, and at the same time, call it making a living. Yet here we are.
Fear of Doctors is real and life threatening. And if Doctors don't receive better training and better education, then these fears will continue to kill people, and not just from the lack of good training and a good education.
Never Events (medical errors) - Patient Doctor Relationships
Women Doctors are better then Male Doctors, it's proven statistically and from my own personal experience, women doctors are more likely to consistently follow established medical procedures; other research has shown that women doctors are more likely to provide preventative care than male ones, and that they are more likely to prescribe medication effectively. And on top of that, you’re more likely to die in a hospital under the care of a male doctor than a woman doctor. Women News.
Several common Causes for Diagnostic Errors include inadequate collaboration and communication among clinicians, patients, and their families. Limited feedback to doctors about the accuracy of diagnoses. A culture that discourages transparency and disclosure of diagnostic errors, which impedes attempts to learn and improve in the medical community.
Informed Consent (right to know)
To Err Is Human is a report that brought the issues of medical error and patient safety to the forefront of national concern. Building a Safer Health System is a landmark report issued in November 1999 by the U.S. Institute of Medicine that may have resulted in increased awareness of U.S. medical errors. The push for patient safety that followed its release continues. The report was based upon analysis of multiple studies by a variety of organizations and concluded that between 44,000 to 98,000 people die each year as a result of preventable medical errors. For comparison, fewer than 50,000 people died of Alzheimer's disease and 17,000 died of illicit drug use in the same year. The report called for a comprehensive effort by health care providers, government, consumers, and others. Claiming knowledge of how to prevent these errors already existed, it set a minimum goal of 50 percent reduction in errors over the next five years. Though not currently quantified, as of 2007 this ambitious goal has yet to be met.
Hospital Infections (super bugs)
Decision Support Center (common ground) - Shared Decisions (mayo clinic)
Collaborate (problem solving)
Objective Structured Clinical Examination (training) - Improve Diagnosis
Shared Decision-Making is an approach in which clinicians and patients communicate together using the best available evidence when faced with the task of making decisions. Patients are supported to deliberate about the possible attributes and consequences of options, to arrive at informed preferences in making a determination about the best course of action which respects patient autonomy, as well as ethical and legal norms.
12 Questions every Patient should ask Doctors and Nurses
1. After admission, ask the names of your primary hospital doctor and the other specialists who make up your physician team. Your primary hospital physician will coordinate with the team, and your nurses will assist you during your stay.
2. Ask your physician: What is my main diagnosis, and are there any other newly diagnosed issues? Feel free to express your fears and anxieties about your diagnosis to the physicians and nursing staff. Don’t let the anxiety build until it becomes uncontrollable.
3. Ask your nurse or physician: How are my illnesses responding to treatment? Ask the nursing staff in particular about how your condition is progressing and how you can facilitate your recovery. It’s your fundamental right to obtain information regarding your medical condition. Understanding both your diagnosis and your treatment plan is a central tenet of the Patient’s Bill of Rights, which was adopted by the Association of American Physicians and Surgeons in 1995. According to this document, all patients are entitled “to be informed about their medical condition, the risks and benefits of treatment, and appropriate alternatives.” Number Needed to Treat.
4. Ask your family, friends, or other trusted individuals to be involved and help support you in your recovery. Yes, it’s hard to put ourselves in a situation where we feel like we’re burdening someone or losing our independence, even for a little while. Understand that these people are an integral part of your treatment team and contribute to the success of your recovery.
5. Ask to speak with a hospital social worker if you have questions about insurance and billing related to your stay. The social worker is there to help clarify what your insurance covers and how much you may be required to pay. If you need assistance with payment, discuss the options available to you with the social worker before you leave as well.
6. Ask to see the nurse manager or charge nurse if you’re experiencing ongoing issues with care or communication about your condition. The person in this role is responsible for helping patients and easing any misunderstanding or tensions that may arise during your stay.
7. As you approach discharge, ask if you should continue taking any of the medications (including vitamins and supplements) you took before you were admitted. This information should be included in your discharge instructions, but take the time to fully understand this aspect of your care to avoid potentially disastrous or even fatal complications later.
8. Ask the staff to show you and your caregivers how to perform any tasks prescribed for after you’ve left the hospital, especially any treatments that may require a special skill, such as changing a bandage or giving an injection. Ask the nurse or physician to remain in your room while you practice to ensure you’re doing it correctly.
9. Ask your nurse or physician if it’s safe to perform ordinary tasks alone, like bathing, dressing, driving, or exercising. Make sure you’ve arranged for help with any of these activities before you leave the hospital.
10. Ask your nurse or physician if you can or should use any medical equipment, such as a walker, brace, or health monitor, to help with your recovery and comfort. If the answer is yes, ask for assistance in obtaining these items before you leave or shortly after your return home.
11. At the time of your discharge, ask the discharge nurse any questions you have about your discharge information. You should have been provided with printed discharge instructions. Don’t leave the hospital without obtaining these, reading them (or having them read to you), and making sure you understanding all of the information they cover.
12. Ask about any follow-up appointments or additional testing. Take a moment now to record anything that’s already been scheduled or to schedule necessary appointments in the coming weeks.
Evidence Based Medicine
Evidence-Based Practice is considering the best available research evidence bearing on whether and why a treatment works, (2) clinical expertise (clinical judgment and experience) to rapidly identify each patient's unique health state and diagnosis, their individual risks and benefits of potential interventions, and (3) client preferences and values. Evidence-based behavioral practice (EBBP) "entails making decisions about how to promote health or provide care by integrating the best available evidence with practitioner expertise and other resources, and with the characteristics, state, needs, values and preferences of those who will be affected. This is done in a manner that is compatible with the environmental and organizational context. Evidence is research findings derived from the systematic collection of data through observation and experiment and the formulation of questions and testing of hypotheses". Pharmaceutical Research Studies.
Duty of Care - Evidence Based Medicine (personalized)
Evidence-Based Nursing is an approach to making quality decisions and providing Nursing Care based upon personal clinical expertise in combination with the most current, relevant research available on the topic. This approach is using evidence based practice (EBP) as a foundation. EBN implements the most up to date methods of providing Care, which have been proven through appraisal of high quality studies and statistically significant research findings. The goal of EBN is to improve the health and safety of patients while also providing care in a cost-effective manner to improve the outcomes for both the patient and the healthcare system. EBN is a process founded on the collection, interpretation, appraisal, and integration of valid, clinically significant, and applicable research. The evidence used to change practice or make a clinical decision can be separated into seven levels of evidence that differ in type of study and level of quality. To properly implement EBN, the knowledge of the nurse, the patient’s preferences, and multiple studies of evidence must all be collaborated and utilized in order to produce an appropriate solution to the task at hand. These skills are taught in modern nursing education and also as a part of professional training.
Evidence-Based Practices (harvard)
Comparative Effectiveness Research is the direct comparison of existing health care interventions to determine which work best for which patients and which pose the greatest benefits and harms. The core question of comparative effectiveness research is which treatment works best, for whom, and under what circumstances.
Agency for Healthcare Research and Quality is to produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable, and to work within the U.S. Department of Health and Human Services and with other partners to make sure that the evidence is understood and used.
Translational Medicine is to combine disciplines, resources, expertise, and techniques within these pillars to promote enhancements in prevention, diagnosis, and therapies. Accordingly, translational medicine is a highly interdisciplinary field, the primary goal of which is to coalesce assets of various natures within the individual pillars in order to improve the global healthcare system significantly. aims to expedite the discovery of new diagnostic tools and treatments by using a multi-disciplinary, highly collaborative, "bench-to-bedside" approach. Within public health, translational medicine is focused on ensuring that proven strategies for disease treatment and prevention are actually implemented within the community. Two roadblocks in need of improvement, the first translational block (T1) prevents basic research findings from being tested in a clinical setting; the second translational block (T2) prevents proven interventions from becoming standard practice.
Medicines and Healthcare Products Regulatory Agency is responsible for ensuring that medicines and medical devices work and are acceptably safe.
National Institute for Health and Care Excellence publishes guidelines in four areas: the use of health technologies within the NHS (such as the use of new and existing medicines, treatments and procedures); clinical practice (guidance on the appropriate treatment and care of people with specific diseases and conditions); guidance for public sector workers on health promotion and ill-health avoidance; and guidance for social care services and users. These appraisals are based primarily on evaluations of efficacy and cost–effectiveness in various circumstances.
Patient Decision Aids (Ottawa Hospital Research Institute)
Shared Decision Making (Informed Medical Decisions)
Transitional Care refers to the coordination and continuity of health care during a movement from one healthcare setting to either another or to home, called care transition, between health care practitioners and settings as their condition and care needs change during the course of a chronic or acute illness. Older adults who suffer from a variety of health conditions often need health care services in different settings to meet their many needs. For young people the focus is on moving successfully from child to adult health services.
Customized Care - Personalized Medicine
Personal Care - Personalized Diet - Racial Bias in Health Care - Racism - Women's Medicine Differences
Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD) ( 2003 )
Racial and Ethnic Disparities in Emergency Department Analgesic Prescription - Implicit (harvard)
Prestige Patient customized care.
The Total Transparency Manifesto - Physicians for Social Responsibility
Echo - Lifelong learning and guided practice model that revolutionizes medical education.
Health Leads is a national healthcare organization that connects low-income patients with the basic resources they need to be healthy. Health Leads intends for healthcare providers to routinely take into account the social and economic reasons people get sick.
Errors - Unnecessary Treatments
Medical Error is a preventable adverse effect of care, whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment. Globally, it is estimated that 142,000 people died in 2013 from adverse effects of medical treatment; this is an increase from 94,000 in 1990. However, a 2016 study of the number of deaths that were a result of medical error in the U.S. placed the yearly death rate in the U.S. alone at 251,454 deaths, which suggests that the 2013 global estimation may not be accurate.
Drug Error's (big pharma)
Diagnostic Error is the leading cause of medical malpractice claims in the US, and is estimated to cause 40,000-80,000 deaths annually. One in every ten diagnoses is wrong and one in every thousand ambulatory diagnostic encounters result in harm.
Never Events are the kind of mistakes that should never happen, especially in the field of medical treatment. Most errors in medical care are clearly identifiable, preventable, and serious in their consequences for patients, which indicates a real problem in the safety and credibility of a health care facility. Never Events are defined as adverse events that are serious and largely preventable, and of concern to both the public and health care providers for the purpose of public accountability.
The number of “adverse events” occurring at Connecticut hospitals rose 7 percent in 2018, compared with the Rate of error in the previous year, with a growing number of patients suffering serious injury or death associated with falls, according to a new state report. Click through to see how many errors or "adverse events" happened at CT hospitals in 2018.
Hospital Readmission is when a patient who had been discharged from a hospital is admitted again to that hospital or another hospital within a specified time frame. The original hospital stay is often called the "index admission" and the subsequent hospital stay is called the "readmission." Different time frames have been used for research purposes, the most common being 30-day, 90-day, and 1-year readmissions. Some researchers start counting days from the date of discharge from the index admission, while other researchers begin counting from the day of a procedure or operation during the index admission. An episode when a patient who had been discharged from a hospital is admitted again within a specified time interval. Readmission rates have increasingly been used as an outcome measure in health services research and as a quality benchmark for health systems. Hospital readmission rates were formally included in reimbursement decisions for the Centers for Medicare and Medicaid Services (CMS) as part of the Patient Protection and Affordable Care Act (ACA) of 2010, which penalizes health systems with higher than expected readmission rates through the Hospital Readmission Reduction Program. Since the inception of this penalty, there have been other programs that have been introduced, with the aim to decrease hospital readmission. The Community Based Care Transition Program, Independence At Home Demonstration Program, and Bundled Payments for Care Improvement Initiative are all examples of these programs. While many time frames have been used historically, the most common time frame is within 30 days of discharge, and this is what CMS uses.
Over Diagnosis is the diagnosis of disease that will never cause symptoms or death during a patient's lifetime. Overdiagnosis is a side effect of screening for early forms of disease. Although screening saves lives in some cases, in others it may turn people into patients unnecessarily and may lead to treatments that do no good and perhaps do harm.
Millions of people get tests, drugs, and operations that won’t make them better, may cause harm, and cost billions.
What if we Paid Doctors to keep People Healthy? Matthias Müllenbeck (video and text) - In the United States, up to 30 percent of all surgical procedures were conducted although other nonsurgical treatment options had not been fully exploited by the physician in charge.
More than 600,000 patients underwent a treatment they didn't need, treatments that collectively cost an estimated $282 million. More than a third of the money spent on the 47 tests or services went to unnecessary care. 3 in 4 annual cervical cancer screenings were performed on women who had adequate prior screenings – at a cost of $19 million. About 85 percent of the lab tests to prep healthy patients for low-risk surgery were unnecessary – squandering about $86 million. Needless annual heart tests on low-risk patients consumed $40 million. Waste Calculator - Health Care Waste in Washington State.
Medical Guidelines may be Biased and Overly Aggressive in US. You don't really hear about people having colonoscopies as a screening procedure in the U.K. It's much less invasive to test for blood in the stool. It's also less costly and doesn't have the risks of undertaking a colonoscopy.
Choosing Wisely seeks to advance a national dialogue on avoiding unnecessary medical tests, treatments and procedures Promoting conversations between patients and clinicians.
30 Percent of all Health Spending — $750 billion — is wasted on fraud, administration and needless procedures. Mammograms needed is overblown. As many as five fewer deaths for 1,000 women. Number Needed to Treat.
Spending on Emergency Room Fees has increased by $3 billion and most hospitals do not make these fees public. Facility Fee is the price of walking through the door and seeking service. It does not include any care provided.
Health Care Cost Institute - Hospitals are now a racket, just like war is a racket, more ways to tax the poor.
Treating Patients in the ER costs, on average, $600 to $1,200 per visit, compared with $165 to $262 if the patients were treated in an outpatient clinic. Last year, the Houston Fire Department logged more than 318,000 incidents, but only thirteen percent of them were actual fires.
"People are receiving inadequate information, education and advice on managing their health." Upstreamists.
Who's My Doctor
Rate your Doctor and Hospital
Patient Safety
Medical Malpractice is professional negligence by act or omission by a health care provider in which the treatment provided falls below the accepted standard of practice in the medical community and causes injury or death to the patient, with most cases involving medical error. Claims of medical malpractice, when pursued in US courts, are processed as civil torts. Sometimes an act of medical malpractice will also constitute a criminal act, as in the case of the death of Michael Jackson. Medical professionals may obtain professional liability insurances to offset the costs of lawsuits based on medical malpractice. Further establishment of conditions of intention or malice may be applied where applicable.
85,000 Paid Medical Malpractice Claims against MDs and DOs in 2001 in the U.S.
Doctors who failed to recognize accurately diagnose and treat the symptoms that ended in injury or death due to the negligence of a physician. When women suffer injuries because of medical negligence, they have a right to be compensated for damages including pain and suffering, lost wages, medical and rehabilitation expenses and more.
Patient Abuse or neglect is any action or failure to act which causes unreasonable suffering, misery or harm to the patient. Abuse includes physically striking or sexually assaulting a patient. It also includes the intentional withholding of necessary food, physical care, and medical attention. Neglect includes the failure to properly attend to the needs and care of a patient, or the unintentional causing of injury to a patient, whether by act or omission. Patient abuse and neglect may occur in settings
such as hospitals, nursing homes, clinics and during home-based care.
Young women still may be getting unnecessary pelvic exams. Millions of 'outdated' tests being performed on healthy females 15 to 20 years old. Pelvic examinations and cervical cancer screenings are no longer recommended for most females under age 21 during routine health visits, but a new study has found that millions of young women are unnecessarily undergoing the tests, which can lead to false-positive testing, over-treatment, anxiety and needless cost. Researchers at UC San Francisco and the Centers for Disease Control and Prevention (CDC) estimated that 1.4 million pelvic examinations and 1.6 million Pap tests performed on U.S. females 15 to 20 years old in a single year may have been medically unnecessary. The findings suggest that despite professional guidelines and recommendations against routine pelvic examinations and Pap tests in this age group, there's a critical lag in clinical practice. The estimated cost of these unnecessary exams was approximately $123 million a year. The investigators estimated that of approximately 2.6 million young women who received a pelvic exam during the previous year, more than half (54.4 percent) were potentially unnecessary, representing an estimated 1.4 million young women. Additionally, the researchers found that nearly a fifth of females younger than the recommended age had a Pap test within the past year. Because 72 percent were performed as "part of a routine exam," they were potentially unnecessary, representing an estimated 1.6 million young women. Almost all of the pelvic examinations were performed at the same time as the Pap test. Young women who had been screened for a sexually transmitted infection were 3.8 times more likely to receive a Pap test and 60 percent more likely to receive a pelvic examination, compared with those who had not been screened. Similarly, young women who used a hormonal contraception other than IUD were 75 percent more likely to receive a Pap test and 31 percent more likely to receive a pelvic examination, compared with those who did not use those contraception methods.This study suggests that healthcare providers and young women need to communicate clearly and often about the best time for these tests.
Intelliguard - RFID solutions for the pharmaceutical and healthcare industries.
Federation of State Medical Boards (wiki) - FSMB
Health Care Systems Four Basic Models
The Association for Medical Education in Europe
Health Records
Medical Scribe is a person, or paraprofessional, who specializes in charting physician-patient encounters in real time, such as during medical examinations. Depending on which area of practice the scribe works in, the position may also be called clinical scribe, ER scribe or ED scribe (in the emergency department), or just scribe (when the context is implicit). A scribe is trained in health information management and the use of health information technology to support it. A scribe can work on-site (at a hospital or clinic) or remotely from a HIPAA-secure facility. Medical scribes who work at an off-site location are known as virtual medical scribes and normally work in clinical settings.
Medical Devices - Medical Implant Warnings
Medical Devices can be easily approved without human testing using loopholes provided by the FDA's 510K product approval process. Pre market approval can be easily manipulated, especially knowing that the FDA has fired scientists for voicing concerns about a products safety. When medical companies do their own research or fund research, they can easily skew the results and facts and also be biased and say things that are not true. FDA approves Cancer causing Chemicals to be in Foods.
If a product is the newest greatest thing, it means that there's very little data and not enough research about how safe the product is. So the product is not yet proven safe. Innovation does not always mean an advancement, because many products do fail and get recalled. And on top of that, Doctors will always have very little experience with a new products, so the risk of a medical mistake is even higher. 70 million Americans have medical devices implanted in their bodies, and there a thousands of horror stories and debilitating complications that have ruined peoples lives. So please be aware and please do your research. Computer Chip in your Brain.
Doctors received over 2 billion dollars in Kickbacks from medical companies in 2016. So when a Doctor says the product is 99% safe, they are not speaking from experience, they are just repeating what the company paid them to say. Always ask your Doctor how many procedures they have done, and if they think they are an expert. 50,000 people a year get cancer from CT Scans, so don't believe for a second that any technology is safe.
Check if your Doctor is getting kickbacks from medical companies, if so, then the doctors decisions can be easily corrupted by money, which could put you at risk of suffering complications.
Always get a second opinion from not just other doctors, but from other sources who have no incentive to lie to you or mislead you. Open Secrets.org - Have you been Harmed in a Medical Facility, please Share your Story.
You have a responsibility to yourself, to maintain a healthy mind and body. To love yourself this way is to reward yourself for loving life. To love life is to be willing to spend some time on the maintenance of life, a maintenance that helps increase the quantity and the quality of life. Maintenance is its own reward. And part of the maintenance is to keep learning. If you are not increasing your knowledge and understanding about life, then life becomes vulnerable and you will not know enough in order to react accurately to the changes that life throws at you. All life forms perform maintenance, and maintenance is a small price to pay for life, it's totally worth the investment.
Risk Factors (risk taking) - Surgical Risk Calculator - Risk Factors in Surgery
The Bleeding Edge Documentary. A searing exposé of the medical device industry from Academy Award-nominated filmmakers Kirby Dick and Amy Ziering.
Readmission Rates
Hospital Readmission Rates are the percentage of admitted patients who return to the hospital within seven days of discharge. In 2016 the readmission rate of 13.9. Readmission rates as an important indicator of the quality of care because they reflect the breadth and depth of care a patient receives. Unnecessary readmissions are also expensive, costing the U.S. $25 billion annually, by one estimate. The Affordable Care Act (ACA) established the Hospital Readmission Reduction Program (HRRP) in 2012. Under this program, hospitals are financially penalized if they have higher than expected risk-standardized 30-day readmission rates for acute myocardial infarction, heart failure, and pneumonia. 10 Ways to Reduce Hospital Readmissions: Understand which patient populations are at greatest risk of readmissions. Target patients with limited English proficiency. Participate in incentive programs with payors. Join a readmission prevention-focused collaborative. Ensure patients schedule a seven-day follow-up. Implement a robust home healthcare program.
Relapse - Recidivism - Prisoner Rehabilitation - Prevention - Intervention
Preventive Services Task Force
Incorporating Patient-Reported Outcomes Into Health Care To Engage Patients And Enhance Care.
Patient-Reported Outcome or PRO is a method or questionnaire used in a clinical trial or a clinical setting, where the responses are collected directly from the patient.
Patient-centered Outcomes are outcomes from medical care that are important to patients.
"Knowledge is the Best Medicine, but you need to do your homework to maximize the benefits"
Remember, fewer than 25 percent of physicians believe they have sufficient training to talk to patients about diet or physical activity. Meanwhile, a good number of physicians are overweight and don't exercise regularly themselves.
Tulane's Medical School is one of the first to teach medical students how to cook healthful food, with the goal that they'll share that knowledge with patients.
Resources for Advancements in Medicine
ASA Physical Status Classification System (wiki)
ASA Physical Status Classification System
Partners In Health
Optum Health Care
Equity Research and Innovation Center (ERIC) Vulnerable and Diverse Populations.
Pioneer Health Foundation
Social Medicine
Health Media Collaboratory
Nutrition Gap, are Doctors ready think outside the Pillbox?
Rock Health full-service funding healthcare entrepreneurs.
Latif Nasser: the amazing story of the man who gave us modern pain relief (video and text)
Bj Miller: What really matters at the end of life (video and text)
Quest Center Empowering people, nurturing community, promoting health and wellbeing.
Robert Wood Johnson Foundation to improve the health and health care of all Americans.
Learners Digest educational and research products for physicians, healthcare professionals, researchers and scientists.
Lasker Foundation Awards Program since 1945 has recognized the contributions of scientists, physicians, and public servants who have made major advances in the understanding, diagnosis, treatment, and prevention of human disease.
Hospital-Acquired Conditions Update, Saving Lives and Saving Money
Hospital-Acquired Condition is an undesirable situation or condition that affects a patient and that arose during a stay in a hospital or medical facility.
Interim estimates for 2014 show a sustained 17 percent decline in hospital-acquired conditions since 2010. A cumulative total of 2.1 million fewer HACs were experienced by hospital patients over the 4 years (2011, 2012, 2013, and 2014) relative to the number of HACs that would have occurred if rates had remained steady at the 2010 level. The measured interim rate for 2014 held steady from 2013 at 121 HACs per 1,000 discharges, down from 145 in 2010. We estimate that nearly 87,000 fewer patients died in the hospital as a result of the reduction in HACs and that approximately $19.8 billion in health care costs were saved from 2010 to 2014.
The federal government is penalizing 758 hospitals with higher rates of patient safety incidents, and more than half of those places had also been fined last year in 2014.
HAC-Reduction-Program - (HAC) Reduction Program
Elderly Abuses (care giving)
Centers for Medicare and Medicaid Services (wiki)
Health Insurance Portability and Accountability Act (wiki)
The CDC has reported that urinary tract infections caused by catheters became slightly more prevalent through 2013.
PSI is a global health organization dedicated to improving the health of people in the developing world by focusing on serious challenges like a lack of family planning, HIV and AIDS, barriers to maternal health, and the greatest threats to children under five, including malaria, diarrhea, pneumonia and malnutrition.
PSI Impact - IHME Institute for Health Metrics and Evaluation
Path global health innovation across five platforms—vaccines, drugs, diagnostics, devices, and system and service innovations.
Human Factors Analysis (PDF) - Common Cause Analysis (PDF)
National Quality Registry Network - American Medical Association
Global Network of institutions and committed individuals whose mission is to Strengthen Health Systems
Physicians for Human Rights - Oaths of Service - Ethics
Skepticism - Skeptic - Questioning - Quack Watch - Pseudoscientific
Medical Malpractice Payout Statistics
Medical Harm: Patient Perceptions and Follow up Actions
Surgical Never Events in the United States. A total of 9,744 paid malpractice settlement and judgments for surgical never events occurring between 1990 and 2010. Malpractice payments for surgical never events totaled $1.3 billion.
Health Care Fraud - Health Care Abuse
Medicare and Medicaid fraudsters are beating taxpayers out of an estimated $90 billion a year - $60 billion of it from Medicare - using a billing scam that is surprisingly easy to execute. CBS And you wonder why Health Care Reform is so important.
The National Council Against Health Fraud - Consumer Protection from Fraud.
Insurance Fraud is any act committed to defraud an insurance process. This occurs when a claimant attempts to obtain some benefit or advantage they are not entitled to, or when an insurer knowingly denies some benefit that is due. According to the United States Federal Bureau of Investigation, the most common schemes include: premium diversion, fee churning, asset diversion, and workers compensation fraud. Perpetrators in these schemes can be insurance company employees or claimants. False insurance claims are insurance claims filed with the fraudulent intention towards an insurance provider. Insurance fraud has existed since the beginning of insurance as a commercial enterprise. Fraudulent claims account for a significant portion of all claims received by insurers, and cost billions of dollars annually. Types of insurance fraud are diverse, and occur in all areas of insurance. Insurance crimes also range in severity, from slightly exaggerating claims to deliberately causing accidents or damage. Fraudulent activities affect the lives of innocent people, both directly through accidental or intentional injury or damage, and indirectly as these crimes lead to higher insurance premiums. Insurance fraud poses a significant problem, and governments and other organizations try to deter such activity.
62% of all Bankruptcies are Related to Medical Bills from people Being Overcharged by greedy hospitals, and on top of that, almost 70% of those people had insurance. So medical fraud is everywhere in many different forms, so no one is safe.
Beware of the Charge Master. Why does Surgery costs differ from town to town?
2.8 Trillion is the estimated cost of Health Care in the US in 2013. Profit over People. America spends more on healthcare than any other country on the planet and millions are still dying and suffering from poor medical care. There are countries who are spending less money and resources on healthcare but have a higher quality healthcare system than the USA.
Drug Errors - Patient Safety - Elderly Abuse
Time Magazine Article "Bitter Pill" - Corporate Terrorism
Why are Doctors allowed to charge insurance companies for unnecessary tests, and also charge to give patients unnecessary drugs. But when a patient needs certain medical care, it's not covered and the patient is forced to pay out of pocket. WTF? It's like you have to be a criminal in order to get help, or to be covered. So who's more criminal, the doctors or the insurance companies?
Bernie Sanders Delivers ‘Major’ Speech on "Medicare for All" | NowThis (youtube) George Washington University July 17th, 2019.
GlaxoSmithKline estimates that 90 percent of the drugs work in only 30 to 50 percent of the people. 300 people have to take the drug statin for a year before one heart attack, stroke or other adverse event is prevented. And five percent of those 300 have side effects, that's 15 people. So you're 15 times more likely to be harmed by the drug than you are to be helped by the drug. There are other ways to reduce your cholesterol that will not harm you.
For the most widely performed surgery on men over the age of 50, removal of the prostate for cancer, the Number Needed to Treat is 49. That means that 49 surgeries are done for every one person who's helped. And the side effects in that case occur in 50 percent of the patients. They include impotence, erectile dysfunction, urinary incontinence, rectal tearing, fecal incontinence. And if you're lucky, and you're one of the 50 percent who has these, they'll only last for a year or two.
Centers for Medicare and Medicaid Services officials chose to do just 30 in-depth financial audits to recover overpayments each year, even though the records make clear they could complete many more, up to 80 audits a year. So only 5 percent of the roughly 600 Medicare Advantage contracts in force would be audited in a year. But overspending tied to fast-rising risk scores has cost taxpayers billions of dollars in recent years, as the Center for Public Integrity reported in a series of articles published in 2014, leading to widespread suspicions that some risk scores are being purposefully inflated. Many of the records released by CMS are heavily redacted, with dates and the names of their authors sometimes missing. More than 1,400 pages have been "withheld in their entirety" by CMS, including names of the health plans and how much they were overpaid. It's like we have criminals watching criminals. If we pay more people to over see and to look for fraud, we could save billions. So we can create thousands of jobs that pay for themselves.
Government Accountability Office Audit: Feds Failed To Rein In Medicare Advantage Overbilling. Private Medicare Advantage plans treating the elderly have overbilled the government by billions of dollars, but rarely been forced to repay the money or face other consequences for their actions, according to a congressional audit.
Insurance - Health Insurance
Insurance is a means of protection from financial loss. It is a form of risk management primarily used to hedge against the risk of a contingent or uncertain loss. Savings - Backup Plan - Securities - Prevention.
Assurance is a promise that a person will be protected and given assistance and help when needed. No one should be denied help or be left behind to suffer. Everyone deserves to live with confidence that their fellow human being will not let them down.
Health Insurance is insurance that covers the whole or a part of the risk of a person incurring medical expenses, spreading the risk over a large number of persons. By estimating the overall risk of health care and health system expenses over the risk pool, an insurer can develop a routine finance structure, such as a monthly premium or payroll tax, to provide the money to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization such as a government agency, private business, or not-for-profit entity. According to the Health Insurance Association of America, health insurance is defined as "coverage that provides for the payments of benefits as a result of sickness or injury. It includes insurance for losses from accident, medical expense, disability, or accidental death and dismemberment".
Insurance is a two-party contract between the insured and the insurance company. The insurance policy assumes a guaranteed promise that the insured will be compensated by the insurance company in the case of a covered loss. A Surety bond is a contract among at least three parties. That means they have a business license, have the proper insurance and have made payments to a surety company for protection by a bond. The insurance company or surety company will be responsible for covering any financial losses. For example: The bond may also cover damage or theft that occurs.
Surety in finance, a surety bond or guaranty involves a promise by one party to assume responsibility for the debt obligation of a borrower if that borrower defaults. The person or company providing the promise is also known as a "surety" or as a "guarantor".
Surety Bond is a promise by a surety or guarantor to pay one party (the obligee) a certain amount if a second party (the principal) fails to meet some obligation, such as fulfilling the terms of a contract. The surety bond protects the obligee against losses resulting from the principal's failure to meet the obligation.
Medical bills is one of the biggest causes of U.S. bankruptcies. Two-thirds of people who file for bankruptcy say medical bills or other issues related to illness contributed to their financial downfall. For middle-class Americans, health insurance sometimes offers little protection. You can wipe out medical debt in Chapter 7 bankruptcy. Hospitals suing people for unpaid medical bills is at an all time high in 2019. Doctor eases your ills with pills only to kill you with bills.
This Doctors Group Is Owned by a Private Equity Firm and Repeatedly Sued the Poor Until We Called Them. After the Blackstone Group acquired one of the nation’s largest physician staffing firms in 2017, low-income patients faced far more aggressive debt collection lawsuits. They only stopped after ProPublica and MLK50 asked about it.
What is the point of having insurance when the insurance claim that you make is denied and not paid or covered? Insurance companies spend more money on fighting claims than paying them.
Health Insurance does not mean better care or better health. Good health mostly comes from acquiring valuable knowledge, information and experience, which is called preventive medicine. And Health Insurance does not guarantee good care because 9 out of 10 Doctors and Dentists commit insurance fraud by doing unnecessary work. So too many Doctors victimize their patients by not giving them the best care that they need, mostly because they are more concerned with how much money they can bilk the insurance carrier for, and not paying attention to the persons needs. So Health Insurance can actually be bad for you, especially when you don't have a good experienced and educated Doctor who is also honest, so be very careful. Medical Errors is the 3rd biggest killer. Does having insurance cause people to take more risks?
Health Inequity is the unfair, uneven distribution of health or health resources. Avoidable differences arising from poor governance, corruption or cultural exclusion. Inequality - Affordable Care Act.
VIP Medicine is when a very important person uses his or her status to influence a given professional or institution to make unorthodox decisions under the pressure or presence of said VIP—that relates to the accessibility and quality of health care. It is essentially health care in which a physician or hospital accommodates a wealthy, important or famous patient who can afford to pay the full medical bill outright, usually with luxury amenities, and seclusion from the ordinary run of patient, as added benefits. As a result, such a patient may receive something other than the normal standard of care; the deviation may be in the direction of either greater or lesser safety and quality.
Medicaid is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance Association of America describes Medicaid as "a government insurance program for persons of all ages whose income and resources are insufficient to pay for health care." Medicaid is the largest source of funding for medical and health-related services for people with low income in the United States, providing free health insurance to 74 million low-income and disabled people (23% of Americans) as of 2017. It is a means-tested program that is jointly funded by the state and federal governments and managed by the states, with each state currently having broad leeway to determine who is eligible for its implementation of the program. States are not required to participate in the program, although all have since 1982. Medicaid recipients must be U.S. citizens or qualified non-citizens, and may include low-income adults, their children, and people with certain disabilities. Poverty alone does not necessarily qualify someone for Medicaid. The Patient Protection and Affordable Care Act (PPACA) significantly expanded both eligibility for and federal funding of Medicaid. Under the law as written, all U.S. citizens and qualified non-citizens with income up to 133% of the poverty line, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program. However, the Supreme Court of the United States ruled in National Federation of Independent Business v. Sebelius that states do not have to agree to this expansion in order to continue to receive previously established levels of Medicaid funding, and some states have chosen to continue with pre-ACA funding levels and eligibility standards. Research suggests that Medicaid improves health insurance coverage, access to health care, recipients' financial security, and some health outcomes, as well as economic benefits to states and health providers. Medicaid and Medicare are the two government sponsored medical insurance programs in the United States and are administered by the U.S. Centers for Medicare & Medicaid Services in Baltimore, Maryland.
Medicare is a national health insurance program in the United States, begun in 1966 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the Social Security Administration, as well as people with end stage renal disease and amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease). In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals—more than 52 million people aged 65 and older and about 8 million younger people. According to annual Medicare Trustees reports and research by the government's MedPAC group, Medicare covers about half of healthcare expenses of those enrolled. Enrollees almost always cover most of the remaining costs by taking additional private insurance and/or by joining a public Part C or Part D Medicare health plan. No matter which of those two options the beneficiaries choose—or if they choose to do nothing extra (around 1% according to annual Medicare Trustees reports over time), beneficiaries also have other healthcare-related costs. These additional so-called out of pocket (OOP) costs can include deductibles and co-pays; the costs of uncovered services—such as for long-term custodial, dental, hearing, and vision care; the cost of annual physical exams for those not on Part C health plans that include physicals; and the costs related to basic Medicare's lifetime and per-incident limits. Medicare is funded by a combination of a specific payroll tax, beneficiary premiums and surtaxes from beneficiaries, co-pays and deductibles, and general U.S. Treasury revenue. Medicare is divided into four Parts. Medicare Part A covers hospital (inpatient, formally admitted only), skilled nursing (only after being formally admitted to a hospital for three days and not for custodial care), and hospice services. Part B covers outpatient services including some providers' services while inpatient at a hospital, outpatient hospital charges, most provider office visits even if the office is "in a hospital", and most professionally administered prescription drugs. Part D covers mostly self-administered prescription drugs. Part C is an alternative called Managed Medicare which allows patients to choose health plans with at least the same service coverage as Parts A and B (and most often more), often the benefits of Part D, and always an annual out-of-pocket spend limit which A and B lack. A beneficiary must enroll in Parts A and B first before signing up for Part C.
The Peckham Experiment (guaranteed income) - Disability Insurance
The best insurance you can have is prevention. Because in order to avoid sickness you have to do all the things that prevent illness. Insurance does not prevent illness or injury, in fact, insurance might encourage illness and injury because people are given a false sense of security and thus fail to take the proper measures that would improve their health, like eating the right foods, exercising and avoiding toxins and viruses. In 2009 there were 48.6 million people in the US (15.7% of the population) who were without Health Insurance Coverage.
Supplemental Insurance is extra or additional insurance that you can purchase to help you pay for services and out-of-pocket expenses that your regular insurance does not cover. Other supplemental plans may provide you with a cash benefit paid out over a period of time or given to you in one lump sum.
"Insurance is knowing someone who is intelligent, someone you can trust"
"The purpose of insurance is not just about money, it's about having a well thought out Backup Plan.
"if things don't turn out the way you wanted, you should have a backup plan, an alternate option, what choices do you have?"
The Affordable Care Act. or Obamacare.
Every human has the right to have the assurance that money gives. No human should ever be without money or be abused because they have no money. Our system is flawed, corrupted and abusive, and it does not need to be that way.
Pre-Obama-Care study found that lack of Health Insurance Killed roughly 45,000 Americans Annually. And the lack of knowledge and information kills millions every year.
Medicaid Expansion Boosts Employment. Individuals with disabilities saw greater working rates in expansion states.
The U.S. Preventive Services Task Force say the link between medical recommendations and insurance coverage leads to financial incentives that can corrupt the process and distort people's health care decisions.
Each year, 1 in every 20 Americans racks up just as much in medical bills as another 19 combined. This critical five percent of the U.S. population is key to solving the nation's health care spending crisis. The United States spends the most on health care per person — $9,237 – according to two new papers published in the journal The Lancet. The U.K. spends less per person ($3,749) on health care than the U.S. ($9,237). Despite its high spending, the U.S. does not have the best health outcomes. Life expectancy, for example, is 79.1 years in the U.S. and 80.9 years in the U.K. And while the U.S. spends more on health care than any country in the world, it ranks 12th in life expectancy among the 12 wealthiest industrialized countries, according to the Kaiser Family Foundation, a non-profit organization focusing on health issues.
Claims Adjuster investigates insurance claims by interviewing the claimant and witnesses, consulting police and hospital records, and inspecting property damage to determine the extent of the company's liability. Verify an insurance policy exists for the insured person and/or property. In general, these are written by the policy-holding insurance company. Risk(s) of loss(es), or damages to property, culminating in the loss of property and or bodily injury. After completing the above investigations, evaluate the covered injuries and/or damages that have been determined according to the coverage grants. Negotiate a settlement according to the applicable law(s), and identify coverage's for which the insured is covered, following best insurance practices.
Professional Liability Insurance or Errors and Omissions, is a form of liability insurance which helps protect professional advice- and service-providing individuals and companies from bearing the full cost of defending against a negligence claim made by a client, and damages awarded in such a civil lawsuit. The coverage focuses on alleged failure to perform on the part of, financial loss caused by, and error or omission in the service or product sold by the policyholder. These are causes for legal action that would not be covered by a more general liability insurance policy which addresses more direct forms of harm. Professional liability insurance may take on different forms and names depending on the profession, especially medical and legal, and is sometimes required under contract by other businesses that are the beneficiaries of the advice or service. Coverage sometimes provides for the defense costs, including when legal action turns out to be groundless. Coverage does not include criminal prosecution, nor a wide range of potential liabilities under civil law that are not enumerated in the policy, but which may be subject to other forms of insurance. Professional liability insurance is required by law in some areas for certain kinds of professional practice.
Liability Insurance is a part of the general insurance system of risk financing to protect the purchaser (the "insured") from the risks of liabilities imposed by lawsuits and similar claims. It protects the insured in the event he or she is sued for claims that come within the coverage of the insurance policy. Originally, individual companies that faced a common peril formed a group and created a self-help fund out of which to pay compensation should any member incur loss (in other words, a mutual insurance arrangement). The modern system relies on dedicated carriers, usually for-profit, to offer protection against specified perils in consideration of a premium. Liability insurance is designed to offer specific protection against third-party insurance claims, i.e., payment is not typically made to the insured, but rather to someone suffering loss who is not a party to the insurance contract. In general, damage caused intentionally as well as contractual liability are not covered under liability insurance policies. When a claim is made, the insurance carrier has the duty (and right) to defend the insured. The legal costs of a defense normally do not affect policy limits unless the policy expressly states otherwise; this default rule is useful because defense costs tend to soar when cases go to trial. In many cases, the defense portion of the policy is actually more valuable than the insurance, as in complicated cases, the cost of defending the case might be more than the amount being claimed, especially in so-called "nuisance" cases where the insured must be defended even though no liability is ever brought to trial.
High-Deductible Health Policies Linked To Delayed Diagnosis And Treatment
Deductible is the amount paid out of pocket by the policy holder before an insurance provider will pay any expenses. Deductibles are typically used to deter the large number of claims that a consumer can be reasonably expected to bear the cost of. By restricting its coverage to events that are significant enough to incur large costs, the insurance firm expects to pay out slightly smaller amounts much less frequently, incurring much higher savings.
Rising Out-of-Pocket Costs of $30 or $40 is a factor of how often a person sees a doctor. Using data from an insurer that provides health coverage to about 20 million people per year across the United States, Ganguli and colleagues found that visits to primary care providers made by adults under the age of 65 had dropped by nearly 25% from 2008 to 2016. What's more, adults who went at least a year without a single visit to a primary care provider increased from about 38% to 46% in that period.
Out-of-Pocket Expense is the direct payment of money that may or may not be later reimbursed from a third-party source.
Negotiate Medical Bills. Always call your medical provider to negotiate medical bills. ask about any wavers, discounts and relief plans or no interest payment plans that are available.
Fair Health Consumer - Estimate your healthcare expenses. Get essential information on costs for thousands of procedures and learn insurance basics.
Healthcare Bluebook - Save money by choosing high-quality, affordable healthcare providers.
Copayment is a fixed amount for a covered service, paid by a patient to the provider of service before receiving the service. It may be defined in an insurance policy and paid by an insured person each time a medical service is accessed. It is technically a form of coinsurance, but is defined differently in health insurance where a coinsurance is a percentage payment after the deductible up to a certain limit. It must be paid before any policy benefit is payable by an insurance company. Copayments do not usually contribute towards any policy out-of-pocket maxima whereas coinsurance payments do. Insurance companies use copayments to share health care costs to prevent moral hazard. It may be a small portion of the actual cost of the medical service but is meant to deter people from seeking medical care that may not be necessary (e.g., an infection by the common cold). In health systems with prices below the market clearing level in which waiting lists act as rationing tools, copayment can serve to reduce the welfare cost of waiting lists. However, a copay may also discourage people from seeking necessary medical care and higher copays may result in non-use of essential medical services and prescriptions, thus rendering someone who is insured effectively uninsured because they are unable to pay higher copays. Thus, there is a balance to be achieved: a high enough copay to deter unneeded expenses but low enough to not render the insurance useless.
Reimbursement is the act of compensating someone for an out-of-pocket expense by giving them an amount of money equal to what was spent.
Co-Insurance is the splitting or spreading of risk among multiple parties.
Cost Sharing occurs when patients pay for a portion of health care costs not covered by health insurance.
Who Still Doesn't have Health Insurance? - Healthcare Act.
Self-Insurance describes a situation in which a person does not take out any third party insurance. The essence of the concept is that a business that is liable for some risk, such as health costs, chooses to "carry the risk" itself and not take out insurance through an insurance company. Preventive Medicine.
Buying Insurance is a form of gambling where the house always wins. All gambling is designed so that the house (i.e. the casino owners or big insurance companies) will always net a profit, regardless of the successes of the patrons. All their games are designed to make you lose more money than you earn, so that the house always wins.
Approximately 12 million adults who seek outpatient medical care are misdiagnosed.
Patient Safety - Elderly and Insurance
Choosing Wisely - Comparing and Rating Healthcare Services
Health Insurance Portability and Accountability Act was created primarily to modernize the flow of healthcare information, stipulate how Personally Identifiable Information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and address limitations on healthcare insurance coverage.
The Association for Community Affiliated Plans (ACAP) is a national trade association representing 60 not-for-profit Safety Net Health Plans in 24 states. Collectively, ACAP plans serve more than fifteen million enrollees, representing more than 50 percent of individuals enrolled in Medicaid-focused health plans.
Insurance Fraud is any act committed to defraud an insurance process. This occurs when a claimant attempts to obtain some benefit or advantage they are not entitled to, or when an insurer knowingly denies some benefit that is due. According to the United States Federal Bureau of Investigation, the most common schemes include: premium diversion, fee churning, asset diversion, and workers compensation fraud. Perpetrators in these schemes can be insurance company employees or claimants. False insurance claims are insurance claims filed with the fraudulent intention towards an insurance provider. Hard fraud occurs when someone deliberately plans or invents a loss, such as a collision, auto theft, or fire that is covered by their insurance policy so they can claim payment for damages. Criminal rings are sometimes involved in hard fraud schemes that can steal millions of dollars. Soft fraud, which is far more common than hard fraud, is sometimes also referred to as opportunistic fraud. This type of fraud consists of policyholders exaggerating otherwise-legitimate claims. For example, when involved in an automotive collision an insured person might claim more damage than actually occurred. Soft fraud can also occur when, while obtaining a new health insurance policy, an individual misreports previous or existing conditions to obtain a lower premium on the insurance policy. The detection of insurance fraud generally occurs in two steps. The first step is to identify suspicious claims that have a higher possibility of being fraudulent. the next step is to refer these claims to investigators for further analysis. Due to the sheer number of claims submitted each day, it would be far too expensive for insurance companies to have employees check each claim for symptoms of fraud. Instead, many companies use computers and statistical analysis to identify suspicious claims for further investigation. There are two main types of statistical analysis tools used: supervised and unsupervised. In both cases, suspicious claims are identified by comparing data about the claim to expected values. The main difference between the two methods is how the expected values are derived. 19 states require mandatory insurer fraud plans. This requires companies to form programs to combat fraud and in some cases to develop investigation units to detect fraud. Split billing is the division of a bill for service into two or more parts. Bills may be split to divide work between clients, payers or for reimbursement to different service providers for performing a shared service. Add-on codes are additional work associated with a primary service or procedure. Add-on codes can and should only be billed when the provider has performed and billed the primary service. CMS guidelines and coding textbooks agree that add-on codes should be on the same claim as the primary code.
Warranty is a promise which is not a condition of the contract or an innominate term: (1) it is a term "not going to the root of the contract", and (2) which only entitles the innocent party to damages if it is breached: i.e. the warranty is not true or the defaulting party does not perform the contract in accordance with the terms of the warranty. A warranty is not a guarantee. It is a mere promise. It may be enforced if it is breached by an award for the legal remedy of damages. A warranty is a term of a contract. Depending on the terms of the contract, a product warranty may cover a product such that a manufacturer provides a warranty to a consumer with which the manufacturer has no direct contractual relationship. A warranty may be express or implied. An express warranty is expressly stated (typically, written); whether or not a term will be implied into a contract depends on the particular contract law of the country in question. Warranties may also state that a particular fact is true at one point in time or that the fact will continue into the future (a "continuing warranty").
Vital Signs - Health Indicators - Biomarkers
Vital Signs or vitals are a group of the four to six most important medical signs that indicate the status of the body’s vital life-sustaining functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person’s vital signs vary with age, weight, gender, and overall health. There are four primary vital signs: body temperature, blood pressure, pulse or heart rate, and breathing rate or respiratory rate, often notated as BT, BP, HR, and RR. However, depending on the clinical setting, the vital signs may include other measurements called the "fifth vital sign" or "sixth vital sign". Vital signs are recorded using the LOINC internationally accepted standard coding system. Early warning scores have been proposed that combine the individual values of vital signs into a single score. This was done in recognition that deteriorating vital signs often precede cardiac arrest and/or admission to the intensive care unit. Used appropriately, a rapid response team can assess and treat a deteriorating patient and prevent adverse outcomes.
Health Indicator are quantifiable characteristics of a population which researchers use as supporting evidence for describing the health of a population. Know your Baseline.
In-Home Mentoring Systems (telemedicine) - Institute for Health Metrics and Evaluation
Examinations - Intelligence - Heart - Blood Pressure
Vitality (nutrition) - Body Fat Index (BMI) - Breathing Measuring (oxygen levels)
Homeostasis is the property of a system in which variables are regulated so that internal conditions remain stable and relatively constant.
Biomarkers are key molecular or cellular events that link a specific environmental exposure to a health outcome. Biomarkers play an important role in understanding the relationships between exposure to environmental chemicals, the development of chronic human diseases, and the identification of subgroups that are at increased risk for disease. Much progress has been made in identifying and validating new biomarkers that can be used in population-based studies of environmental disease.
Biomarker is a measurable indicator of some biological state or condition. Biomarkers are often measured and evaluated to examine normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention. Biomarkers are used in many scientific fields.
Bio-Monitoring (Body Burden)
Biomarkers of Aging are biomarkers that could predict functional capacity at some later age better than chronological age. Stated another way, biomarkers of aging would give the true "biological age", which may be different from the chronological age.
Validated biomarkers of aging would allow for testing interventions to extend lifespan, because changes in the biomarkers would be observable throughout the lifespan of the organism. Although maximum lifespan would be a means of validating biomarkers of aging, it would not be a practical means for long-lived species such as humans because longitudinal studies would take far too much time. Ideally, biomarkers of aging should assay the biological process of aging and not a predisposition to disease, should cause a minimal amount of trauma to assay in the organism, and should be reproducibly measurable during a short interval compared to the lifespan of the organism. An assemblage of biomarker data for an organism could be termed its "ageotype".
Although graying of hair increases with age, hair graying cannot be called a biomarker of ageing. Similarly, skin wrinkles and other common changes seen with aging are not better indicators of future functionality than chronological age. Biogerontologists have continued efforts to find and validate biomarkers of aging, but success thus far has been limited. Levels of CD4 and CD8 memory T cells and naive T cells have been used to give good predictions of the expected lifespan of middle-aged mice. Advances in big data analysis allowed for the new types of "aging clocks" to be developed. The epigenetic clock is a promising biomarker of aging and can accurately predict human chronological age. Basic blood biochemistry and cell counts can also be used to accurately predict the chronological age. Further studies of the hematological clock on the large datasets from South Korean, Canadian, and Eastern European populations demonstrated that biomarkers of aging may be population-specific and predictive of mortality. It is also possible to predict the human chronological age using the transcriptomic clock. The recent introduction of low-power and compact sensors, based on micro-electromechanical systems (MEMS) has led to a new breed of the wearable and affordable devices providing unparalleled opportunities for the collecting and cloud-storing personal digitized activity records. Consequently, modern deep machine learning techniques could be used to produce a proof-of-concept digital biomarker of age in the form of all-causes-mortality predictor from a sufficiently large collection of one week long human physical activity streams augmented by the rich clinical data (including the death register, as provided by, e.g., the NHANES study).
Grip Strength and Mortality - Longevity
Biological Age is a measurement of your age based on various biomarkers — a number that can change due to lifestyle and other health factors. Knowing your biological age is an effective way of determining your cumulative rate of aging.
Smartphone Medical Apps - Analyzing Tools (sensors)
A new way to Monitor Vital Signs (that can see through walls): Dina Katabi (video and text)
Biometrics is the technical term for body measurements and calculations. It refers to metrics related to human characteristics. Biometrics authentication (or realistic authentication) is used in computer science as a form of identification and access control. It is also used to identify individuals in groups that are under surveillance. Biometric identifiers are the distinctive, measurable characteristics used to label and describe individuals. Biometric identifiers are often categorized as physiological versus behavioral characteristics. Physiological characteristics are related to the shape of the body. Examples include, but are not limited to fingerprint, palm veins, face recognition, DNA, palm print, hand geometry, iris recognition, retina and odour/scent. Behavioral characteristics are related to the pattern of behavior of a person, including but not limited to typing rhythm, gait, and voice. Some researchers have coined the term behaviometrics to describe the latter class of biometrics. More traditional means of access control include token-based identification systems, such as a driver's license or passport, and knowledge-based identification systems, such as a password or personal identification number. Since biometric identifiers are unique to individuals, they are more reliable in verifying identity than token and knowledge-based methods; however, the collection of biometric identifiers raises privacy concerns about the ultimate use of this information.
Wellness - Well Being - Health Assessments
Wellness is the level of functional and metabolic efficiency of a living organism. In humans it is the ability of individuals or communities to adapt and self-manage when facing physical, mental or social challenges. In Good Health.
Physical Wellness encompasses nutrition, physical fitness and the avoidance of unhealthy habits like smoking, drinking too much and doing drugs. Fitness Assessment.
Screening - Examinations - Prevention - Vital Signs - Blood Pressure
Intellectual Wellness - Mental Wellness dimension refers to the amount of information and knowledge you take in, and the amount of creative, analytical thinking you put out. Learning, problem solving and mental productivity are important aspects of intellectual wellness.
Emotional Wellness - Spiritual Wellness pertains to how well you are aware of, accepting of and able to deal with your feelings. Relationships, stress, self-esteem and life outlook are all factors that play into emotional wellness. It can make you feel more resilient.
Medical Wellness involves health-promoting medical practices like medical check-ups, preventative healthcare and medical health management.
Wellness Alternative means a healthy balance of the mind, body and spirit that results in an overall feeling of well-being.
Quality of Life (satisfaction and fulfillmernt)
Wellness Coach - Wellness Coaches
Rockford Wellness Center - Wellness Study in the Workplace (PDF)
Occupational wellness stresses the importance of a positive attitude towards work, and a rewarding and enriching career path.
Nutrition (food knowledge) - Preventative Health
Health Indicator are quantifiable characteristics of a population which researchers use as supporting evidence for describing the health of a population. Typically, researchers will use a survey methodology to gather information about certain people, use statistics in an attempt to generalize the information collected to the entire population, then use the statistical analysis to make a statement about the health of the population.
Public Health Intervention is any effort or policy that attempts to improve mental and physical health on a population level.
Mental Health Assessments - Interventions
Health Assessment is a plan of care that identifies the specific needs of a person and how those needs will be addressed by the healthcare system or skilled nursing facility. Health assessment is the evaluation of the health status by performing a physical exam after taking a health history. It is done to detect diseases early in people that may look and feel well. Evidence does not support routine health assessments in otherwise healthy people. Health assessment is the evaluation of the health status of an individual along the health continuum. The purpose of the assessment is to establish where on the health continuum the individual is because this guides how to approach and treat the individual. The health care approaches range from preventive, to treatment, to palliative care in relation to the individual's status on the health continuum. It is not the treatment or treatment plan. The plan related to findings is a care plan which is preceded by the specialty such as medical, physical therapy, nursing, etc.
Integrative Healing Center healing program for body, mind, and spirit, which combines conventional medicine along with alternative forms of healing to allow for complete restoration of the human body that is naturally designed to heal itself when given the proper balance of nutrition, sunlight, rest and relaxation, and detoxification. Cancer.
Health is the level of functional and metabolic efficiency of a living organism. In humans it is the ability of individuals or communities to adapt and self-manage when facing physical, mental or social challenges.
Well-Being is a contented state of being happy and healthy and prosperous. Includes choices and activities aimed at achieving physical vitality, mental alacrity, social satisfaction, a sense of accomplishment, and personal fulfillment. An individual or a group's condition is positive, while low well-being is associated with negative happenings. Factors which are key for well-being are Self-acceptance, Personal growth, Purpose in life, Environmental mastery, Autonomy, Positive relations with others.
Workplace Wellness is any workplace health promotion activity or organizational policy designed to support healthy behavior in the workplace and to improve health outcomes. Workplace Safety.
Workplace Health Promotion is the combined efforts of employers, employees, and society to improve the mental and physical health and well-being of people at work. The term workplace health promotion denotes a comprehensive analysis and design of human and organizational work levels with the strategic aim of developing and improving health resources in an enterprise.
Workplace Democracy is the application of democracy in various forms (examples include voting systems, debates, democratic structuring, due process, adversarial process, systems of appeal) to the workplace.
Wellness Alternative Medicine a healthy balance of the mind, body and spirit that results in an overall feeling of well-being.
Physical Education - Think Well, Act Well, Feel Well, Be Well - Live, Learn, Love and Progress.
Universal access to Physical Activity could save Billions in Health Costs
Environmental Wellness relates to your level of environmental consciousness. Remember that every cell in your body was created by elements from the environment through the food you eat, what you drink and breathe. Your well-being is intertwined with the well-being of the environment.
Social Wellness has to do with how you see your place in the world and in society, and how well you adjust to your personal role in society.
How To Create a Wellness Program (youtube)
Lawson Health Research Institute understands the basis of wellness and the dysfunctions of the body and mind that result in disease.
Health Calculators - How Healthy are You
Medical Calculator is a type of medical computer software, whose purpose is to allow easy calculation of various scores and indices, presenting the user with a friendly interface that hides the complexity of the formulas. Some of the standard units they make include eGFR, CrCl, BMI, BSA, DAS and many other custom units designed for a specific purpose.
Indices is a numerical scale used to compare variables with one another or with some reference number. A number or ratio (a value on a scale of measurement) derived from a series of observed facts; can reveal relative changes as a function of time. A mathematical notation indicating the number of times a quantity is multiplied by itself.
Health Calculator - Health Status Calculators
Health Calculators - Calculate Body Health - Health Calculator
22 Senior Health Risk Calculators for Healthy Aging
Risk of Developing Chronic Diseases - Chronic Diseases - Fatigue
Smartphone Health Monitoring Technology Tools - Tiny Machines
Health Care is the prevention, treatment, and management of illness and the preservation of health through the services offered by health care organizations and professionals. It includes all the goods and services designed to promote health, including “preventive, curative and palliative interventions, whether directed to individuals or to populations.
Measures of Health Status can be measured using pathological and clinical measures and is usually observed by clinicians or measured using instruments. Types of disease measurement include: Signs - blood pressure, temperature, X-ray, tumour size. Symptoms - disease specific checklists. Co-morbidity - Charlson Index, ICED- index of co-existing disease (looks at both disease severity and functional severity), adverse events – pain, bleeding, readmission, complications (e.g. using Clavien-Dindo Classification of Surgical Complications).
Body Mass Index - Body Fat Measurement
Body Mass Index is a measurement of relative weight based on an individual's mass and height. Overweight is defined as a body mass index, or BMI, of 25 to 29.9, which is about ten to 30 pounds overweight depending on your height. Obese is defined as anyone with a BMI of 30 or above.
BMI Calculator (Underweight = <18.5) - (Normal weight = 18.5–24.9) - (Overweight = 25–29.9) - (Obesity = BMI of 30 or greater)
Visceral Fat (obesity) - How Fat Are You?
Normal Weight individuals who Develop type 2 Diabetes: The Personal Fat Threshold.
Doctor Examination Visits (examinations)
Body Burden Test Analysis and Bio-Monitoring
Vitamin Testing
Brainwaves could be the next Health Vital Sign - Vitals.
5 Biomarkers factors that influence Inner Age: Glucose, Vitamin D, Testosterone, hsCRP and ALT.
Abdominal Obesity occurs when excessive abdominal fat around the stomach and abdomen has built up to the extent that it is likely to have a negative impact on health. Central obesity has been strongly linked to cardiovascular disease, Alzheimer's disease, and other metabolic and vascular diseases.
Breathalyzers
Breathalyzer is a device that measures chemicals in a person's expired breath. Breathalyzer (wiki)
Breathalyzer can diagnose 17 different diseases via Pattern Analysis of Exhaled Molecules.
Detecting Disease Through Breath Prof. Hossam Haick Technion (youtube)
Health Calculators - Wellness Testing
Breathing - Lungs - Spirometer - Choking or Not Breathing - O2 Measuring
Na-Nose: A Nanoscale Artificial Nose to Detect Specific Medical Conditions. Volatile organic compounds in exhaled breath, sweat or urine carry much information on the state of human health. Volatile Biomarkers.
Blood Pressure
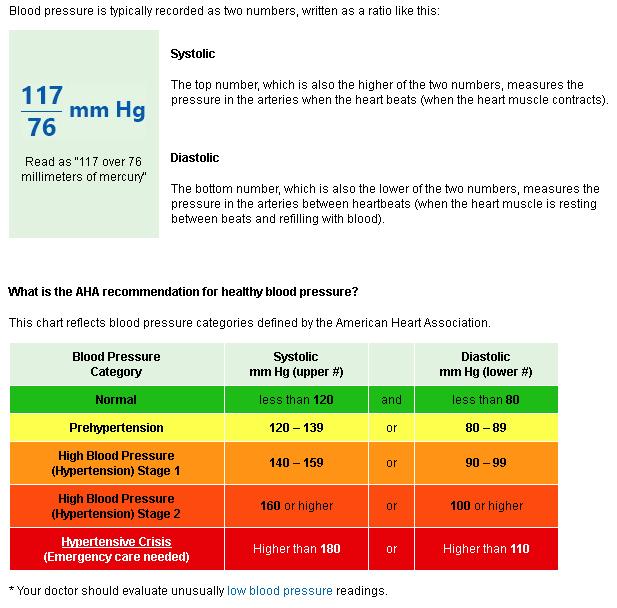 Blood
Pressure is the pressure of circulating
blood on the walls of blood
vessels. Most of this pressure is due to work done by the heart by pumping
blood through the circulatory system. Blood pressure usually refers to the pressure in large arteries of the
systemic circulation. Blood pressure is usually expressed in terms of the
systolic pressure (maximum during one heartbeat) over diastolic pressure
(minimum in between two heartbeats) and is measured in millimeters of
mercury (mmHg), above the surrounding atmospheric pressure. (mm Hg is
Millimeter
of Mercury, which is a
manometric unit of
pressure).
Blood
Pressure is the pressure of circulating
blood on the walls of blood
vessels. Most of this pressure is due to work done by the heart by pumping
blood through the circulatory system. Blood pressure usually refers to the pressure in large arteries of the
systemic circulation. Blood pressure is usually expressed in terms of the
systolic pressure (maximum during one heartbeat) over diastolic pressure
(minimum in between two heartbeats) and is measured in millimeters of
mercury (mmHg), above the surrounding atmospheric pressure. (mm Hg is
Millimeter
of Mercury, which is a
manometric unit of
pressure).Make sure that you are getting an Accurate Blood Pressure Reading you should avoid food, exercise, caffeine, tobacco and alcohol for 30 minutes before taking a measurement. And you should sit quietly and be relaxed with feet flat on the floor before and during monitoring. Don't measure your blood pressure right after you wake up. And make sure you have a normal body temperature. You must also confirm that you have a device that is calibrated and accurate. You should measure your blood pressure twice daily if you can. Sphygmomanometer is a device used to measure blood pressure and a means to determine at what pressure blood flow is just starting, and at what pressure it is unimpeded. Not all BP Devices are the same, so you must know how to use a particular device in order to get an accurate measurement. BP Devices are also known as a blood pressure meter, blood pressure monitor, or blood pressure gauge. The device is composed of an inflatable cuff to collapse and then release the artery under the cuff in a controlled manner, and a mercury or mechanical manometer to measure the pressure. It is always used in conjunction with a means to determine at what pressure blood flow is just starting, and at what pressure it is unimpeded. Manual sphygmomanometers are used in conjunction with a stethoscope. A sphygmomanometer consists of an inflatable cuff, a measuring unit (the mercury manometer, or aneroid gauge), and a mechanism for inflation which may be a manually operated bulb and valve or a pump operated electrically.
A single high blood pressure reading does not necessarily mean that you have high blood pressure. However, if readings stay at 140/90 mm Hg or above (systolic 140 or above OR diastolic 90 or above) over time, your doctor will likely want you to begin a treatment program.
White Coat Hypertension is a phenomenon in which patients exhibit a blood pressure level above the normal range, in a clinical setting, though they don't exhibit it in other settings. Brain Strokes - Oxygen Levels.
High Blood Pressure affects 1.13 billion people around the world while blood pressure has dropped sharply in high-income countries, it has risen in many low and middle-income countries, especially those in Africa and South Asia. Globally, 597 million men had raised blood pressure, compared to 529 million women. High blood pressure puts extra strain on the blood vessels and major organs such as heart, brain and kidneys. It is the world's leading cause of cardiovascular disease, which leads to stroke and heart attacks, and is thought to cause 7.5 million deaths a year across the globe.
High Blood Pressure (hypertension) - 10 ways to control high blood pressure without medication.
Difference in blood pressure between arms linked to greater early death risk. Robust evidence from a large international study confirms that a difference in blood pressure readings between arms is linked to greater risk of heart attack, stroke and death.
Global Disparities of Hypertension Prevalence and Control A Systematic Analysis of Population-Based Studies From 90 Countries says 32 percent of low-income people have high blood pressure, compared with 29 percent in high-income countries. Long term high blood pressure is a major risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease, vision loss, and chronic kidney disease. Blood Pressure Prevalence.
Blood
Blood flows from the Heart through arteries, which branch and narrow into arterioles, and then branch further into capillaries where nutrients and wastes are exchanged. The capillaries then join and widen to become venules, which in turn widen and converge to become veins, which then return blood back to the heart through the venae cavae, which are two large veins (venous trunks) that return deoxygenated blood from the body into the heart. In humans there are the superior vena cava and the inferior vena cava, and both empty into the right atrium. They are located slightly off-center, toward the right side of the body. The right atrium receives deoxygenated blood through coronary sinus and two large veins called Venae Cavae. The inferior vena cava (or caudal vena cava in some animals) travels up alongside the abdominal aorta with blood from the lower part of the body. It is the largest vein in the human body. The superior vena cava (or cranial vena cava in animals) is above the heart, and forms from a convergence of the left and right brachiocephalic veins, which contain blood from the head and the arms.
Artery is a blood vessel that carries blood from the heart to the body.
Vein is a blood vessel that carries blood from the capillaries toward the heart.
Capillary is a small blood vessel from 5 to 10 micrometres (µm) in diameter, and having a wall one endothelial cell thick. They are the smallest blood vessels in the body: they convey blood between the arterioles and venules. These microvessels are the site of exchange of many substances with the interstitial fluid surrounding them. Substances which exit include water (proximal portion), oxygen, and glucose; substances which enter include water (distal portion), carbon dioxide, uric acid, lactic acid, urea and creatinine. Lymph capillaries connect with larger lymph vessels to drain lymphatic fluid collected in the microcirculation. Capillaries are very thin blood vessels that bring nutrients and oxygen to tissues and remove waste products. Inflammation.
Venule is a very small blood vessel in the microcirculation that allows blood to return from the capillary beds to drain into the larger blood vessels, the veins. Venules range from 7μm to 1mm in diameter. Veins contain approximately 70% of total blood volume, 25% of which is contained in the venules. Many venules unite to form a vein.
Blood Vessel are the part of the circulatory system, and microcirculation, that transports blood throughout the human body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and the tissues; and the veins, which carry blood from the capillaries back toward the heart.
Lymphatic Vessel are thin-walled vessels (tubes) structured like blood vessels, that carry lymph. As part of the lymphatic system, lymph vessels are complementary to the cardiovascular system. Lymph vessels are lined by endothelial cells, and have a thin layer of smooth muscle, and adventitia that binds the lymph vessels to the surrounding tissue. Lymph vessels are devoted to the propulsion of the lymph from the lymph capillaries, which are mainly concerned with absorption of interstitial fluid from the tissues. Lymph capillaries are slightly larger than their counterpart capillaries of the vascular system. Lymph vessels that carry lymph to a lymph node are called afferent lymph vessels, and those that carry it from a lymph node are called efferent lymph vessels, from where the lymph may travel to another lymph node, may be returned to a vein, or may travel to a larger lymph duct. Lymph ducts drain the lymph into one of the subclavian veins and thus return it to general circulation. Generally, lymph flows away from the tissues to lymph nodes and eventually to either the right lymphatic duct or the largest lymph vessel in the body, the thoracic duct. These vessels drain into the right and left subclavian veins, respectively. The lymphatic vessels contain valves.
Endothelium is a type of epithelium that lines the interior surface of blood vessels and lymphatic vessels, forming an interface between circulating blood or lymph in the lumen and the rest of the vessel wall. It is a thin layer of simple squamous cells called endothelial cells. Endothelial cells in direct contact with blood are called vascular endothelial cells, whereas those in direct contact with lymph are known as lymphatic endothelial cells. Vascular endothelial cells line the entire circulatory system, from the heart to the smallest capillaries. These cells have unique functions in vascular biology. These functions include fluid filtration, such as in the glomerulus of the kidney, blood vessel tone, hemostasis, neutrophil recruitment, and hormone trafficking. Endothelium of the interior surfaces of the heart chambers is called endocardium.
Hematology is the branch of medicine concerned with the study, diagnosis, treatment, and prevention of diseases related to blood. - Blood Donation.
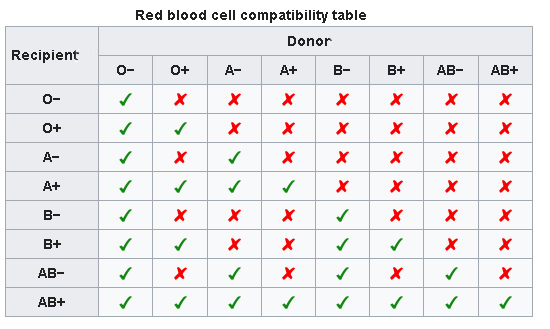 Blood Type is a
classification of blood based on the presence and absence of
antibodies
and also based on the presence or absence of inherited
antigenic
substances on the surface of red blood cells (RBCs). These antigens may be
proteins, carbohydrates, glycoproteins, or glycolipids, depending on the
blood group system. Some of these antigens are also present on the
surface of other types of
cells of various tissues. Several of these red blood cell surface
antigens can stem from one allele (or an alternative version of a gene)
and collectively form a blood group system. Blood types are inherited and
represent contributions from both parents. A total of 35 human blood group
systems are now recognized by the International Society of Blood
Transfusion. The two most important ones are ABO and the RhD
antigen; they determine someone's blood type (A, B, AB and O, with +, − or
Null denoting RhD status). Many pregnant women
carry a fetus with a blood type which is different from their own,
which is not a problem. What can matter is whether the baby is RhD
positive or negative. Mothers who are RhD- and carry a RhD+ baby can form
antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG,
a small immunoglobulin, which can cross the placenta and cause hemolysis
of fetal RBCs, which in turn can lead to hemolytic disease of the newborn
called erythroblastosis fetalis, an illness of low fetal blood counts that
ranges from mild to severe. Sometimes this is lethal for the fetus; in
these cases it is called hydrops fetalis. The
Universal Blood Type is O Negative (O-). Donors with type O- blood
have the unique power to help anyone in need of a blood transfusion. Red
blood cells from O- donors can be transfused to anyone, regardless of the
person's blood type.
Histo-blood
group ABO system transferase is an enzyme with glycosyltransferase
activity, which is encoded by the ABO gene in humans. It is ubiquitously
expressed in many tissues and cell types. ABO determines the ABO blood
group of an individual by modifying the oligosaccharides on cell surface
glycoproteins. Variations in the sequence of the protein between
individuals determine the type of modification and the blood group. The
ABO gene also contains one of 27 SNPs associated with increased risk of
coronary artery disease.
Blood Type is a
classification of blood based on the presence and absence of
antibodies
and also based on the presence or absence of inherited
antigenic
substances on the surface of red blood cells (RBCs). These antigens may be
proteins, carbohydrates, glycoproteins, or glycolipids, depending on the
blood group system. Some of these antigens are also present on the
surface of other types of
cells of various tissues. Several of these red blood cell surface
antigens can stem from one allele (or an alternative version of a gene)
and collectively form a blood group system. Blood types are inherited and
represent contributions from both parents. A total of 35 human blood group
systems are now recognized by the International Society of Blood
Transfusion. The two most important ones are ABO and the RhD
antigen; they determine someone's blood type (A, B, AB and O, with +, − or
Null denoting RhD status). Many pregnant women
carry a fetus with a blood type which is different from their own,
which is not a problem. What can matter is whether the baby is RhD
positive or negative. Mothers who are RhD- and carry a RhD+ baby can form
antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG,
a small immunoglobulin, which can cross the placenta and cause hemolysis
of fetal RBCs, which in turn can lead to hemolytic disease of the newborn
called erythroblastosis fetalis, an illness of low fetal blood counts that
ranges from mild to severe. Sometimes this is lethal for the fetus; in
these cases it is called hydrops fetalis. The
Universal Blood Type is O Negative (O-). Donors with type O- blood
have the unique power to help anyone in need of a blood transfusion. Red
blood cells from O- donors can be transfused to anyone, regardless of the
person's blood type.
Histo-blood
group ABO system transferase is an enzyme with glycosyltransferase
activity, which is encoded by the ABO gene in humans. It is ubiquitously
expressed in many tissues and cell types. ABO determines the ABO blood
group of an individual by modifying the oligosaccharides on cell surface
glycoproteins. Variations in the sequence of the protein between
individuals determine the type of modification and the blood group. The
ABO gene also contains one of 27 SNPs associated with increased risk of
coronary artery disease.Scientists Develop Ingenious Way to Convert Blood Into Universal Donor Type. A new paper presents a viable way to convert type A blood into O blood using enzymes that from the gut bacterium Flavonifractor plautii. When these enzymes are added to type A blood, the molecules on its surface that define it as A type become unattached, turning it into universal type O blood. This is very useful, considering type A positive blood is the second most common type in America, while only 7 percent are universal type O negative donors.
Rh Blood Group System is one of 36 known human blood group systems. It is the second most important blood group system, after the ABO blood group system. The Rh blood group system consists of 49 defined blood group antigens, among which the five antigens D, C, c, E, and e are the most important. There is no d antigen. Rh(D) status of an individual is normally described with a positive or negative suffix after the ABO type (e.g., someone who is A Positive has the A antigen and the Rh(D) antigen, whereas someone who is A Negative lacks the Rh(D) antigen). The terms Rh factor, Rh positive, and Rh negative refer to the Rh(D) antigen only. Antibodies to Rh antigens can be involved in hemolytic transfusion reactions and antibodies to the Rh(D) and Rh(c) antigens confer significant risk of hemolytic disease of the fetus and newborn. Rhesus (Rh) factor is an inherited protein found on the surface of red blood cells. If your blood has the protein, you're Rh positive. If your blood lacks the protein, you're Rh negative. Rh positive is the most common blood type.
Blood Test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using a needle, or via fingerprick. Multiple tests for specific blood components (such as a glucose test or a cholesterol test) are often grouped together into one test panel called a blood panel or blood work. Blood tests are often used in health care to determine physiological and biochemical states, such as disease, mineral content, pharmaceutical drug effectiveness, and organ function. Typical clinical blood panels include a basic metabolic panel or a complete blood count. Blood tests are also used in drug tests to detect drug abuse. In some of the United States, a blood test is required before marriage. DNA.
Complete Blood Count Test gives your doctor important information about the types and numbers of cells in your blood, especially the red blood cells and their percentage (hematocrit) or protein content (hemoglobin), white blood cells, and platelets. The results of a CBC may diagnose conditions like anemia, infection, and other disorders. The platelet count and plasma clotting tests (prothombin time, partial thromboplastin time, and thrombin time) may be used to evaluate bleeding and clotting disorders. Your doctor may also perform a Blood Smear, which is a way of looking at your blood cells under the microscope. In a normal blood smear, red blood cells will appear as regular, round cells with a pale center. Variations in the size or shape of these cells may suggest a blood disorder.
Phlebotomy is the process of making an incision in a vein with a needle. The procedure itself is known as a venipuncture. A person who performs phlebotomy is called a "phlebotomist", although doctors, nurses, medical laboratory scientists and others do portions of phlebotomy procedures in many countries.
Near-Infrared Vein Finder are devices used to try to increase the ability of healthcare providers to see veins. They use near-infrared light reflection to create a map of the veins. The received imagery is then either displayed on a screen or projected back onto the patient's skin. Unsurprisingly, they may not increase the success of starting intravenous catheters in children, since the difficulty may arise not in locating the vessel, but in physical manipulation of the needle.
Measuring blood damage. Engineer uses mechanical resistance to detect damage to red blood cells. Red blood cells sometimes rupture when blood is sent through faulty equipment, such as a dialysis machine. This is called hemolysis. Hemolysis also can occur during blood work when blood is drawn too quickly through a needle, leading to defective laboratory samples. Researchers have now developed a method to monitor blood damage in real-time.
Automated Robotic Device For Faster Blood Testing.
Blood Work Sample (image)
New Blood Test Technology using cellphone-based technology that allows for the very same test to be conducted in the doctor's office, clinic or even in a remote area. A mobile version of the Enzyme Linked Immunosorbent Assay (ELISA), proving a cheap and easy way to obtain bloodwork and urinalysis without visiting a laboratory. ELISA is the gold standard technique used to detect the presence of an antibody or antigen.
Hypovolemia is a state of decreased blood volume or diminished body fluid; more specifically, decrease in volume of blood plasma. It is thus the intravascular component of volume contraction (or loss of blood volume due to things such as bleeding or dehydration), but, as it also is the most essential one, hypovolemia and volume contraction are sometimes used synonymously. Hypovolemia is characterized by sodium depletion, and thus is distinct from (although often overlapping with) dehydration, excessive loss of body water.
Red Blood Cells are the most common type of blood cell in your blood. Blood is the vertebrate organism's principal means of delivering oxygen (O2) to the body tissues—via blood flow through the circulatory system. RBCs take up oxygen in the lungs or gills and release it into tissues while squeezing through the body's capillaries. Red blood cells are produced by cores of bone marrow in the heads of long bones in a process known as hematopoiesis. Hematopoietic stem cells are capable of transforming into red blood cells, white blood cells, and platelets. These stem cells can be found circulating in the blood and bone marrow in people of all ages, as well as in the umbilical cords of newborn babies. Stem cells from all three sources may be used to treat a variety of diseases, including leukemia, lymphoma, bone marrow failure, and various immune disorders. Hemoglobin is the iron-containing oxygen-transport metalloprotein in the red blood cells. Hemoglobin is a red protein responsible for transporting oxygen in the blood of vertebrates. Its molecule comprises four subunits, each containing an iron atom bound to a heme group. Red blood cells absorb lots of blue light and reflects lots of red light. When someone is turning "blue in the face", it means that they're not getting enough oxygen. Production of red blood cells is controlled by erythropoietin, a hormone produced primarily by the kidneys. Red blood cells start as immature cells in the bone marrow and after approximately seven days of maturation are released into the bloodstream. Unlike many other cells, red blood cells have no nucleus and can easily change shape, helping them fit through the various blood vessels in your body. However, while the lack of a nucleus makes a red blood cell more flexible, it also limits the life of the cell as it travels through the smallest blood vessels, damaging the cell's membranes and depleting its energy supplies. The red blood cell survives on average only 120 days. Red cells contain a special protein called hemoglobin, which helps carry oxygen from the lungs to the rest of the body and then returns carbon dioxide from the body to the lungs so it can be exhaled. Blood appears red because of the large number of red blood cells, which get their color from the hemoglobin. The percentage of whole blood volume that is made up of red blood cells is called the hematocrit and is a common measure of red blood cell levels.
Anemia is a condition in which you don't have enough healthy red blood cells to carry adequate oxygen to the body's tissues. Having anemia may make you feel tired and weak. There are many forms of anemia, each with its own cause. Anemia can be temporary or long term, and it can range from mild to severe.
Erythropoietin is a glycoprotein cytokine secreted by the kidney in response to cellular Hypoxia; it stimulates red blood cell production (erythropoiesis) in the bone marrow. Low levels of EPO (around 10 mU/mL) are constantly secreted sufficient to compensate for normal red blood cell turnover. Common causes of cellular hypoxia resulting in elevated levels of EPO (up to 10 000 mU/mL) include any anemia, and hypoxemia due to chronic lung disease.
White Blood Cells are the Cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from multipotent cells in the bone marrow known as hematopoietic stem cells. Leukocytes are found throughout the body, including the blood and lymphatic system.
Monitor Detects Dangerously Low White Blood Cell Levels.
Mast Cell is a type of white blood cell. Specifically, it is a type of granulocyte derived from the myeloid stem cell that is a part of the immune and neuroimmune systems and contains many granules rich in histamine and heparin. Although best known for their role in allergy and anaphylaxis, mast cells play an important protective role as well, being intimately involved in wound healing, angiogenesis, immune tolerance, defense against pathogens, and blood–brain barrier function. The mast cell is very similar in both appearance and function to the basophil, another type of white blood cell. Although mast cells were once thought to be tissue resident basophils, it has been shown that the two cells develop from different hematopoietic lineages and thus cannot be the same cells.
B Cell are a type of white blood cell of the lymphocyte subtype. They function in the humoral immunity component of the adaptive immune system by secreting antibodies. Immune System Cells.
Blood Plasma is a yellowish liquid component of blood that holds the blood cells in whole blood in suspension. It is the liquid part of the blood that carries cells and proteins throughout the body. It makes up about 55% of the body's total blood volume. It is the intravascular fluid part of extracellular fluid (all body fluid outside cells). It is mostly water (up to 95% by volume), and contains dissolved proteins (6–8%) (e.g. serum albumins, globulins, and fibrinogen), glucose, clotting factors, electrolytes (Na+, Ca2+, Mg2+, HCO3−, Cl−, etc.), hormones, carbon dioxide (plasma being the main medium for excretory product transportation) and oxygen. It plays a vital role in an intravascular osmotic effect that keeps electrolyte concentration balanced and protects the body from infection and other blood disorders. Blood plasma is separated from the blood by spinning a tube of fresh blood containing an anticoagulant in a centrifuge until the blood cells fall to the bottom of the tube. The blood plasma is then poured or drawn off. Blood plasma has a density of approximately 1025 kg/m3, or 1.025 g/ml. Blood serum is blood plasma without clotting factors. Plasmapheresis is a medical therapy that involves blood plasma extraction, treatment, and reintegration. Fresh frozen plasma is on the WHO Model List of Essential Medicines, the most important medications needed in a basic health system. It is of critical importance in the treatment of many types of trauma which result in blood loss, and is therefore kept stocked universally in all medical facilities capable of treating trauma (e.g. trauma centers, hospitals, and ambulances) or that pose a risk of patient blood loss such as surgical suite facilities.
Plasma Cell are white blood cells that secrete large volumes of antibodies. They are transported by the blood plasma and the lymphatic system. Plasma cells originate in the bone marrow; B cells differentiate into plasma cells that produce antibody molecules closely modelled after the receptors of the precursor B cell. Once released into the blood and lymph, these antibody molecules bind to the target antigen (foreign substance) and initiate its neutralization or destruction.
Platelet are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus: they are fragments of cytoplasm that are derived from the megakaryocytes of the bone marrow, which then enter the circulation. Circulating unactivated platelets are biconvex discoid (lens-shaped) structures, 2–3 µm in greatest diameter. Activated platelets have cell membrane projections covering their surface. Platelets are found only in mammals, whereas in other vertebrates (e.g. birds, amphibians) thrombocytes circulate as intact mononuclear cells. A higher than normal number of platelets can cause unnecessary clotting, which can lead to strokes and heart attacks; however, thanks to advances made in antiplatelet therapies, there are treatments available to help prevent these potentially fatal events. Conversely, lower than normal counts can lead to extensive bleeding. Unlike red and white blood cells, platelets are not actually cells but rather small fragments of cells. Platelets help the blood clotting process (or coagulation) by gathering at the site of an injury, sticking to the lining of the injured blood vessel, and forming a platform on which blood coagulation can occur. This results in the formation of a fibrin clot, which covers the wound and prevents blood from leaking out. Fibrin also forms the initial scaffolding upon which new tissue forms, thus promoting healing. Platelet Plug is an aggregation of platelets formed during the earlier stage of hemostasis in response to blood vessel wall injury. Cuts and Skin Wounds.
Coagulation or Clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism of coagulation involves activation, adhesion, and aggregation of platelets along with deposition and maturation of fibrin. Disorders of coagulation are disease states which can result in bleeding (hemorrhage or bruising) or obstructive clotting (thrombosis).
Clotting is a thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to prevent bleeding, but can be harmful in thrombosis, when clots obstruct blood flow through healthy blood vessels.
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system.
Bleeding also known as hemorrhaging or hemorrhaging, is blood escaping from the circulatory system. Bleeding can occur internally, where blood leaks from blood vessels inside the body, or externally, either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a break in the skin. Hypovolemia is a massive decrease in blood volume, and death by excessive loss of blood is referred to as exsanguination. Typically, a healthy person can endure a loss of 10–15% of the total blood volume without serious medical difficulties (by comparison, blood donation typically takes 8–10% of the donor's blood volume). The stopping or controlling of bleeding is called hemostasis and is an important part of both first aid and surgery. Vitamin K.
Internal Bleeding is a loss of blood that occurs from a blood vessel and collects inside the body. Internal bleeding is usually not visible from the outside. It is a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding (e.g. heart, brain, stomach, lungs). Severe internal bleeding into the chest, abdomen, retroperitoneum, pelvis, and thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly. Stroke - Aneurysm - Embolism.
Vetigel Stops Bleeding - First Aid (bleeding).
Prothrombin Time is a blood test that measures how long it takes blood to clot. A prothrombin time test can be used to check for bleeding problems. PT is also used to check whether medicine to prevent blood clots is working. This blood test is also called protime INR and PT/INR. They are used to determine the clotting tendency of blood, in the measure of warfarin dosage, liver damage, and vitamin K status. PT measures the following coagulation factors: I (fibrinogen), II (prothrombin), V (proaccelerin), VII (proconvertin), and X (Stuart–Prower factor). The normal range for a healthy person not using warfarin is 0.8–1.2, and for people on warfarin therapy an INR of 2.0–3.0 is usually targeted, although the target INR may be higher in particular situations, such as for those with a mechanical heart valve. INR means International Normalized Ratio.
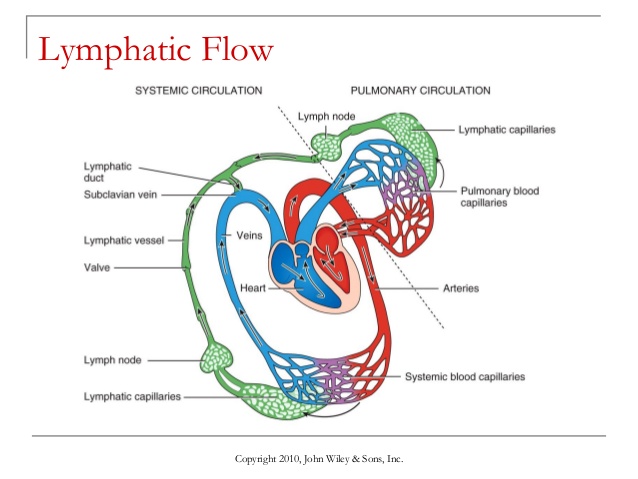 Lymphatic System
is part of the circulatory system and a vital part of the
immune system, comprising a
network of lymphatic vessels that carry a clear fluid called lymph (from
Latin, lympha meaning "water") directionally towards the heart.
Lymphatic System
is part of the circulatory system and a vital part of the
immune system, comprising a
network of lymphatic vessels that carry a clear fluid called lymph (from
Latin, lympha meaning "water") directionally towards the heart.Lymph is the fluid that flows through the lymphatic system, a system composed of lymph vessels (channels) and intervening lymph nodes whose function, like the venous system, is to return fluid from the tissues to the central circulation. Interstitial fluid – the fluid which is between the cells in all body tissues – enters the lymph capillaries. This lymphatic fluid is then transported via progressively larger lymphatic vessels through lymph nodes, where substances are removed by tissue lymphocytes and circulating lymphocytes are added to the fluid, before emptying ultimately into the right or the left subclavian vein, where it mixes with central venous blood. Since the lymph is derived from the interstitial fluid, its composition continually changes as the blood and the surrounding cells continually exchange substances with the interstitial fluid. It is generally similar to blood plasma, which is the fluid component of blood. Lymph returns proteins and excess interstitial fluid to the bloodstream. Lymph also transports fats from the digestive system (beginning in the lacteals) to the blood via chylomicrons. Bacteria may enter the lymph channels and be transported to lymph nodes, where they are destroyed.[clarification needed] Metastatic cancer cells can also be transported via lymph.
Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult person, approximately 10/11–10/12 new blood cells are produced daily in order to maintain steady state levels in the peripheral circulation.
Blood Poisoning is a serious infection. It occurs when bacteria are in the bloodstream. Despite its name, the infection has nothing to do with poison. Although not a medical term, “blood poisoning” is used to describe bacteremia, septicemia, or sepsis. Sepsis is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. Common signs and symptoms include fever, increased heart rate, increased breathing rate, and confusion. There also may be symptoms related to a specific infection, such as a cough with pneumonia, or painful urination with a kidney infection. In the very young, old, and people with a weakened immune system, there may be no symptoms of a specific infection and the body temperature may be low or normal, rather than high. Severe sepsis is sepsis causing poor organ function or insufficient blood flow. Insufficient blood flow may be evident by low blood pressure, high blood lactate, or low urine output. Septic shock is low blood pressure due to sepsis that does not improve after reasonable amounts of intravenous fluids are given. Sepsis is caused by an immune response triggered by an infection. Most commonly, the infection is bacterial, but it may also be from fungi, viruses, or parasites. Common locations for the primary infection include lungs, brain, urinary tract, skin, and abdominal organs. Risk factors include young or old age, a weakened immune system from conditions such as cancer or diabetes, major trauma, or burns. An older method of diagnosis was based on meeting at least two systemic inflammatory response syndrome (SIRS) criteria due to a presumed infection. In 2016, SIRS was replaced with qSOFA which is two of the following three: increased breathing rate, change in level of consciousness, and low blood pressure. Blood cultures are recommended preferably before antibiotics are started, however, infection of the blood is not required for the diagnosis. Medical imaging should be used to look for the possible location of infection. Other potential causes of similar signs and symptoms include anaphylaxis, adrenal insufficiency, low blood volume, heart failure, and pulmonary embolism, among others. Sepsis usually is treated with intravenous fluids and antibiotics. Typically, antibiotics are given as soon as possible. Often, ongoing care is performed in an intensive care unit. If fluid replacement is not enough to maintain blood pressure, medications that raise blood pressure may be used.
Metabolic Waste are substances left over from metabolic processes (such as cellular respiration) which cannot be used by the organism (they are surplus or toxic), and must therefore be excreted. This includes nitrogen compounds, water, CO2, phosphates, sulphates, etc. Animals treat these compounds as excretes. Plants have chemical "machinery" which transforms some of them (primarily the nitrogen compounds) into useful substances.
Oxygen Levels in Blood
Oxygen Saturation is a term referring to the fraction of Oxygen-saturated hemoglobin relative to total hemoglobin (unsaturated + saturated) in the blood. The human body requires and regulates a very precise and specific balance of oxygen in the blood. Normal blood oxygen levels in humans are considered 95-100 percent. If the level is below 90 percent, it is considered low resulting in hypoxemia. Blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Continued low oxygen levels may lead to respiratory or cardiac arrest. Oxygen Therapy may be used to assist in raising blood oxygen levels. Oxygenation occurs when oxygen molecules (O2) enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood. Oxygenation is commonly used to refer to medical oxygen saturation. Oxygen Saturation Monitoring by Pulse Oximetry. Normal oxygen saturation values are 97% to 99% in the healthy individual. Oxygen saturation indicates how much oxygen the blood is carrying as a percentage of the maximum it could carry. Red blood cells contain iron containing protein hemoglobin. Hemoglobin attaches oxygen to the red blood cell and carries it through the body. 1 hemoglobin molecule can attach up to 4 oxygen molecules, which is considered to be 100 percent saturation. A healthy person with healthy lungs and breathing air at sea level, a healthy persons oxygen saturation should be between 95 and 100 percent. The maximum volume of oxygen which the blood can carry when fully saturated is termed the oxygen carrying capacity, which, with a normal haemoglobin concentration, is approximately 20 mL oxygen per 100 mL blood. Blood Pressure.
Pulse Oximetry is a noninvasive method for monitoring a person's oxygen saturation (SO2). Its reading of SpO2 (peripheral oxygen saturation) is not always identical to the reading of SaO2 (arterial oxygen saturation) from arterial blood gas analysis, but the two are correlated well enough that the safe, convenient, noninvasive, inexpensive pulse oximetry method is valuable for measuring oxygen saturation in clinical use. In its most common (transmissive) application mode, a sensor device is placed on a thin part of the patient's body, usually a fingertip or earlobe, or in the case of an infant, across a foot. The device passes two wavelengths of light through the body part to a photodetector. It measures the changing absorbance at each of the wavelengths, allowing it to determine the absorbances due to the pulsing arterial blood alone, excluding venous blood, skin, bone, muscle, fat, and (in most cases) nail polish. Reflectance pulse oximetry may be used as an alternative to transmissive pulse oximetery described above. This method does not require a thin section of the person's body and is therefore well suited to a universal application such as the feet, forehead, and chest, but it also has some limitations. Vasodilation and pooling of venous blood in the head due to compromised venous return to the heart, as occurs with congenital cyanotic heart disease patients, or in patients in the Trendelenburg position, can cause a combination of arterial and venous pulsations in the forehead region and lead to spurious SpO2 results. What are Normal Oxygen Saturation Levels? The normal oxygen saturation level is 97–100%. Older adults typically have lower oxygen saturation levels than younger adults. For example, someone older than 70 years of age may have an oxygen saturation level of about 95%, which is an acceptable level. For example, someone older than 70 years of age may have an oxygen saturation level of about 95%, which is In practice, the SpO2 range of 92–100% is generally acceptable for most clients. It is important to note that the oxygen saturation level varies considerably based on a person’s state of health. Thus, it is important to understand both baseline readings and underlying physiology associated with certain conditions to interpret oxygen saturation levels and changes in these levels. People who are obese and/or have conditions such as lung and cardiovascular diseases, emphysema, chronic obstructive pulmonary disease, congenital heart disease and sleep apnea tend to have lower oxygen saturation levels. Additionally, oxygen saturation levels may decrease slightly when a person is talking. Oxygen saturation may remain normal (e.g., 97% and higher) for people with anemia. However, this may not indicate adequate oxygenation because there are less hemoglobin to carry an adequate supply of oxygen for people who have anemia. The inadequate supply of oxygen may be more prominent during activity for people with anemia. Falsely low oxygen saturation levels may be associated with hypothermia, decreased peripheral perfusion, and cold extremities. In these cases, an ear lobe pulse oximeter device or arterial blood gases would provide a more accurate oxygen saturation level. However, arterial blood gases are usually only taken in critical care or emergency settings. In practice, the SpO2 range of 92–100% is generally acceptable for most clients. Some experts have suggested that a SpO2 level of at least 90% will prevent hypoxic tissue injury and ensure client safety (Beasley, et al., 2016). Blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Normal arterial oxygen is approximately 75 to 100 millimeters of mercury (mm Hg). Values under 60 mm Hg usually indicate the need for supplemental oxygen. Normal pulse oximeter readings usually range from 95 to 100 percent. Values under 90 percent are considered low. The oxygen level from a pulse oximeter is reasonably accurate. Most oximeters give a reading 2% over or 2% under what your saturation would be if obtained by an arterial blood gas. Racial Bias in Pulse Oximetry Measurement can give errors for patients with dark skin.
Breathing - Lungs - Spirometer - Choking or Not Breathing
Physiologic Status Monitoring via the Gastrointestinal Tract (youtube)
Physiologic Status Monitoring via the Gastrointestinal Tract - Microbes
Proteus - Sensor Applications
Photoplethysmogram is an optically obtained plethysmogram that can be used to detect blood volume changes in the microvascular bed of tissue. A PPG is often obtained by using a pulse oximeter which illuminates the skin and measures changes in light absorption. A conventional pulse oximeter monitors the perfusion of blood to the dermis and subcutaneous tissue of the skin.
Photoplethysmography in the assessment of blood flow and vascular mechanics. The biomechanics of blood flow can provide parameters for prediction of cardiovascular diseases CVD at an early stage.
Syncope: Review of Monitoring Modalities - Syncope is the short loss of consciousness and muscle strength.
Health Home Test
Normal Body Temperature is around 37C (98.6F), although it depends on: The person, Their age, What they've been doing, the time of day, and which part of the body you take the temperature from. It is generally accepted that normal body temperature ranges between 36.1C (97F) to 37.2C (99F).
The Human Body - Every Breath You Take
Oxygen therapy harms lung microbiome in mice. We now know that the balance of bacteria inside the lungs matters much like it does in the gut. Oxygen is actually a potent lung toxin. If I put healthy mice in 100% oxygen, they will die in five days.
Oxygen Therapy is the use of oxygen as a medical treatment. This can include for low blood oxygen, carbon monoxide toxicity, cluster headaches, and to maintain enough oxygen while inhaled anesthetics are given.
Our bodies need a certain amount of oxygen molecules circulating in the bloodstream at all times. When all internal organs are functioning correctly, the oxygen that you inhale passes from the tiny alveoli or air sacs of your lungs into the bloodstream, and the pumping action of your heart delivers this oxygenated blood to all parts of your body.
Blood Therapy
Blood Transfusion is generally the process of receiving blood or blood products into one's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors, and platelets.
Platelet-Rich Plasma (cancer) - Synthetic Blood
Every two seconds, an American needs a blood transfusion. But blood transfusions aren’t as simple as taking one person’s blood and giving it to another. There are four different types, but type O negative blood is the only one that can be given to people with all other types. Because of this “universal” quality, it’s in short supply and in high demand, but an incredible breakthrough announced Monday could change that. Longevity.
International Society of Blood Transfusion is a scientific society, founded in 1935, which aims to promote the study of blood transfusion, and to spread the know-how about the manner in which blood transfusion medicine and science best can serve the patient's interests. The society's central office is in Amsterdam, and there are around 1700 members in 97 countries. Currently in 2020, the President is Martin L. Olsson.
At Home Dialysis Machine
Intravenous is within or by means of a vein.
Intravenous Therapy is a therapy that delivers liquid substances directly into a vein (intra- + ven- + -ous). The intravenous route of administration can be used for injections (with a syringe at higher pressures) or infusions (typically using only the pressure supplied by gravity). Intravenous infusions are commonly referred to as drips. The intravenous route is the fastest way to deliver medications and fluid replacement throughout the body, because the circulation carries them. Intravenous therapy may be used for fluid replacement (such as correcting dehydration), to correct electrolyte imbalances, to deliver medications, and for blood transfusions.
Blood Irradiation Therapy is a procedure in which the blood is exposed to low level red light (often laser light) for therapeutic reasons. Most research on blood irradiation therapy has been conducted in Germany (by UV lamps), and in Russia (in all variants) while smaller-scale research has been performed in other countries such as Britain. Blood irradiation therapy can be administered in three ways. Extracorporeally, drawing blood out and irradiating it in a special cuvette. This method is used for the ultraviolet (UV) blood irradiation (UVBI) by UV lamps. The laser light is monochromatic, i.e. it has such a wavelength that allows you to bring light into the optical fiber and carry out irradiation intravenously through a catheter in a vein. This method is more simple and effective. Blood irradiation therapy is also administered externally through the skin on the projection of large blood vessels. It is not related to the practice of gamma irradiation of blood in transfusion medicine.
Saline as a medicine is a mixture of sodium chloride in water and has a number of uses in medicine. Applied to the affected area it is used to clean wounds, help remove contact lenses, and help with dry eyes. By injection into a vein it is used to treat dehydration such as from gastroenteritis and diabetic ketoacidosis. It is also used to dilute other medications to be given by injection. Large amounts may result in fluid overload, swelling, acidosis, and high blood sodium. In those with long-standing low blood sodium, excessive use may result in osmotic demyelination syndrome. Saline is in the crystalloid family of medications. It is most commonly used as a sterile 9 g of salt per litre (0.9%) solution, known as normal saline. Higher and lower concentrations may also occasionally be used. Saline has a pH of 5.5 (mainly due to dissolved carbon dioxide) making it acidic. The salinity (salt concentration) of blood is approximately 0.9% while the salinity of sea water is approximately 3.5%.
Blood Donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation (separation of whole-blood components). Donation may be of whole blood (WB), or of specific components directly (the latter called apheresis). Blood Banks often participate in the collection process as well as the procedures that follow it. As blood plasma, in contrast to blood, can be donated as often as once every 2 weeks.
Blood Plasma is a yellowish coloured liquid component of blood that normally holds the blood cells in whole blood in suspension; this makes plasma the extracellular matrix of blood cells. It makes up about 55% of the body's total blood volume. It is the
intravascular fluid part of extracellular fluid (all body fluid outside cells). It is mostly water (up to 95% by volume), and contains dissolved proteins (6–8%) (i.e.—serum albumins, globulins, and fibrinogen), glucose, clotting factors, electrolytes (Na+, Ca2+, Mg2+, HCO3−, Cl−, etc.), hormones, carbon dioxide (plasma being the main medium for excretory product transportation) and oxygen. Plasma also serves as the protein reserve of the human body. It plays a vital role in an intravascular osmotic effect that keeps electrolytes in balanced form and protects the body from infection and other blood disorders. Blood plasma is separated from the blood by spinning a tube of fresh blood containing an anticoagulant in a centrifuge until the blood cells fall to the bottom of the tube. The blood plasma is then poured or drawn off. Blood plasma has a density of approximately 1025 kg/m3, or 1.025 g/ml. Blood serum is blood plasma without clotting factors.
Chemistry - Hormones
James Harrison (blood donor) also known as the Man with the golden arm, is a blood plasma donor from Australia whose unusual plasma composition has been used to make a treatment for Rhesus disease. He has made over 1000 donations throughout his lifetime, and these donations are estimated to have saved over 2.4 million unborn babies from the condition. As of 4 September 2017, Harrison had donated 1157 times. As Australia has a policy prohibiting blood donations from individuals past age 81, he made his final donation on 11 May 2018. Alloimmunity.
Heart
 Heart is a muscular organ in humans and other animals, which
pumps blood through the blood vessels of the circulatory system. Blood
provides the body with oxygen and
nutrients, as well as assists in
the removal of metabolic wastes. The heart is located in the middle
compartment of the chest behind the
sternum
and between the lungs.
Heart is a muscular organ in humans and other animals, which
pumps blood through the blood vessels of the circulatory system. Blood
provides the body with oxygen and
nutrients, as well as assists in
the removal of metabolic wastes. The heart is located in the middle
compartment of the chest behind the
sternum
and between the lungs.Heart Attack (heart stops beating)
Scientists maps molecular mechanisms crucial for new approach to heart disease therapy. Scientists have reprogrammed ordinary cells called fibroblasts into new and healthy heart muscle cells, and recorded changes that appear to be necessary for this reprogramming.
Heart Disease kills more than 600,000 people each year in the United States alone and remains the leading cause of death for both men and women. Diseases of heart muscle are of major importance. These include conditions caused by a restricted blood supply to the muscle including angina pectoris and myocardial infarction, and other heart muscle disease known as cardiomyopathies.
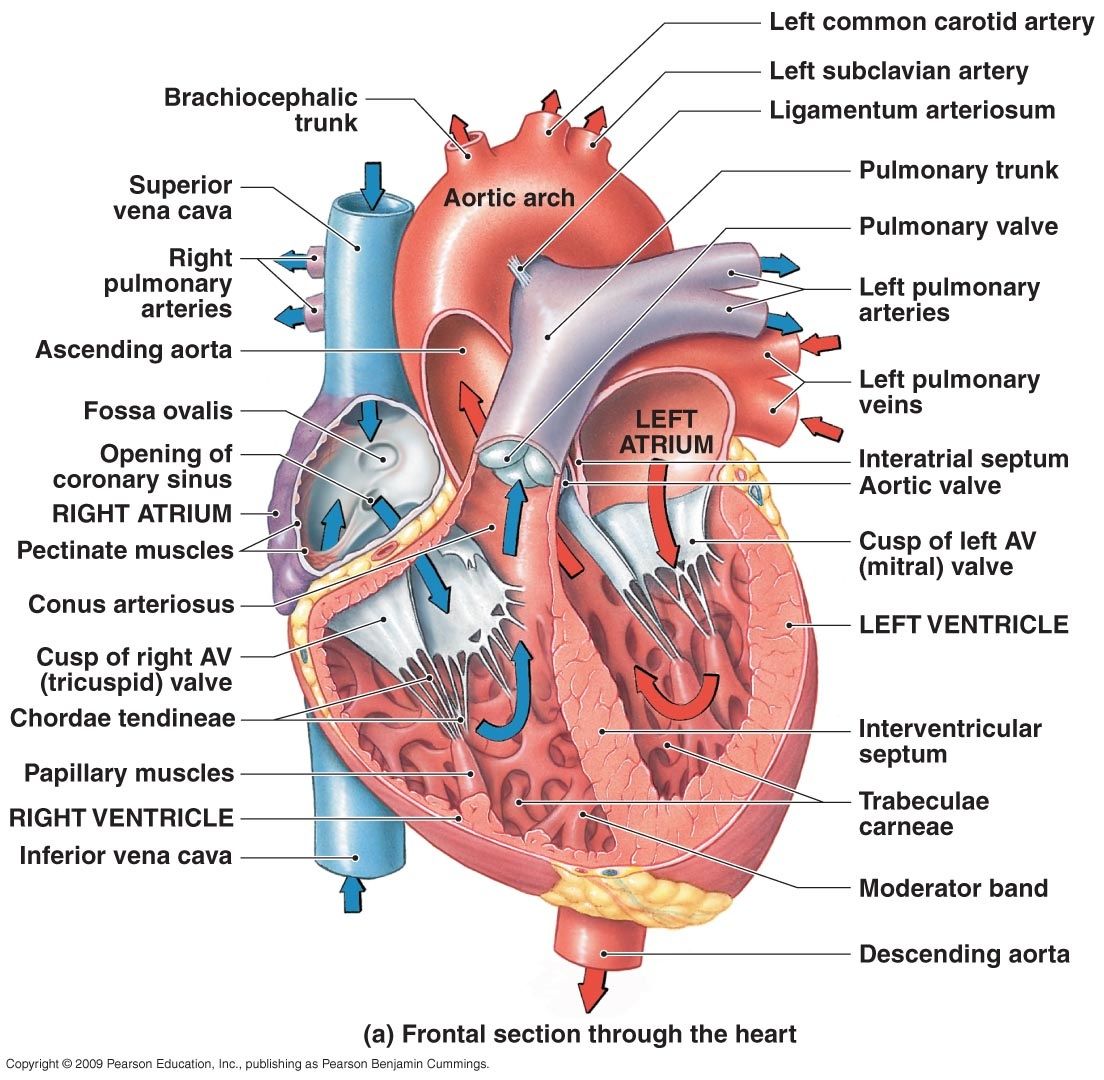 Cardiac Muscle
or heart muscle is one of the three major types of
muscle, the others being
skeletal and smooth muscle. It is an involuntary, striated muscle that is
found in the walls of the heart. This muscle tissue is known as
myocardium, and forms a thick middle layer between the outer layer of the
heart wall (the epicardium) and the inner layer (the endocardium).
Myocardium is composed of individual heart muscle cells (cardiomyocytes)
joined together by intercalated disks, encased by collagen fibres and
other substances forming the extracellular matrix. Cardiac muscle
contracts in a similar manner to skeletal muscle, albeit with some
important differences. An electrical stimulation in the form of an action
potential triggers the release of calcium from the cell's internal calcium
store, the sarcoplasmic reticulum. The rise in calcium causes the cell's
myofilaments to slide past each other in a process called excitation
contraction coupling.
Cardiac Muscle
or heart muscle is one of the three major types of
muscle, the others being
skeletal and smooth muscle. It is an involuntary, striated muscle that is
found in the walls of the heart. This muscle tissue is known as
myocardium, and forms a thick middle layer between the outer layer of the
heart wall (the epicardium) and the inner layer (the endocardium).
Myocardium is composed of individual heart muscle cells (cardiomyocytes)
joined together by intercalated disks, encased by collagen fibres and
other substances forming the extracellular matrix. Cardiac muscle
contracts in a similar manner to skeletal muscle, albeit with some
important differences. An electrical stimulation in the form of an action
potential triggers the release of calcium from the cell's internal calcium
store, the sarcoplasmic reticulum. The rise in calcium causes the cell's
myofilaments to slide past each other in a process called excitation
contraction coupling. Arteries carry the blood away from the heart to be used by the body. Capillaries enable the actual exchange of water and chemicals between the blood and the tissues. Veins carry blood from the capillaries back toward the Heart.
Cardiac Muscle Cell are the muscle cells (myocytes) that make up the cardiac muscle (heart muscle). Each myocardial cell contains myofibrils, which are specialized organelles consisting of long chains of sarcomeres, the fundamental contractile units of muscle cells. Cardiomyocytes show striations similar to those on skeletal muscle cells. Unlike multinucleated skeletal cells, the majority of cardiomyocytes contain only one nucleus, although they may have as many as four. Cardiomyocytes have a high mitochondrial density, which allows them to produce adenosine triphosphate (ATP) quickly, making them highly resistant to fatigue.
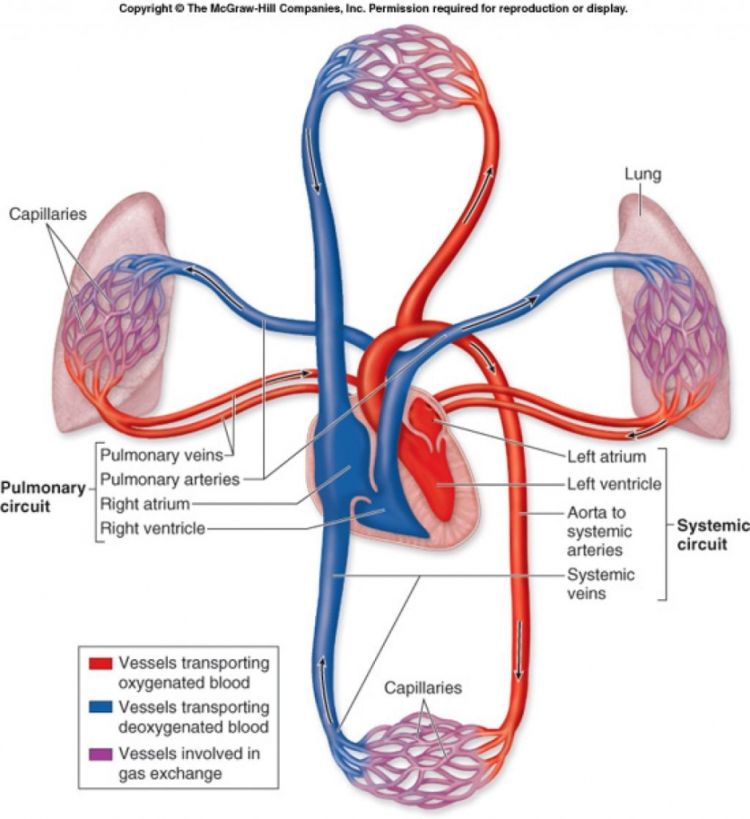 Myocyte is the
type of cell found in muscle
tissue. Myocytes are long, tubular cells that develop from myoblasts
to form muscles in a process known as myogenesis. There are various
specialized forms of myocytes: cardiac, skeletal, and smooth muscle cells,
with various properties. The striated cells of cardiac and skeletal
muscles are referred to as muscle fibers. Cardiomyocytes are the muscle
fibres that form the chambers of the heart, and have a single central
nucleus. Skeletal muscle fibers help support and move the body and tend to
have peripheral nuclei. Smooth muscle cells control involuntary movements
such as the peristalsis contractions in the oesophagus and stomach.
Myofibril (muscles)
Myocyte is the
type of cell found in muscle
tissue. Myocytes are long, tubular cells that develop from myoblasts
to form muscles in a process known as myogenesis. There are various
specialized forms of myocytes: cardiac, skeletal, and smooth muscle cells,
with various properties. The striated cells of cardiac and skeletal
muscles are referred to as muscle fibers. Cardiomyocytes are the muscle
fibres that form the chambers of the heart, and have a single central
nucleus. Skeletal muscle fibers help support and move the body and tend to
have peripheral nuclei. Smooth muscle cells control involuntary movements
such as the peristalsis contractions in the oesophagus and stomach.
Myofibril (muscles)Adenosine Triphosphate is a complex organic chemical that participates in many processes. Found in all forms of life, ATP is often referred to as the "molecular unit of currency" of intracellular energy transfer. When consumed in metabolic processes, it converts to either the di- or monophosphates, respectively ADP and AMP. Other processes regenerate ATP such that the human body recycles its own body weight equivalent in ATP each day. It is also a precursor to DNA and RNA. From the perspective of biochemistry, ATP is classified as a nucleoside triphosphate, which indicates that it consists of three components, a nitrogenous base (adenine), the sugar ribose, and the triphosphate. It is used in cells as a coenzyme.
Circulatory System is an organ system that permits blood to circulate and transport nutrients (such as amino acids and electrolytes), oxygen, carbon dioxide, hormones, and blood cells to and from the cells in the body to provide nourishment and help in fighting diseases, stabilize temperature and pH, and maintain homeostasis. The study of the blood flow is called hemodynamics. The study of the properties of the blood flow is called hemorheology.
Peripheral Circulation is concerned with the transport of blood, blood flow distribution, exchange between blood and tissue, and storage of blood (venous system).
Peripheral Vascular System is the part of the circulatory system that consists of the veins and arteries not in the chest or abdomen (i.e. in the arms, hands, legs and feet). The peripheral arteries supply oxygenated blood to the body, and the peripheral veins lead deoxygenated blood from the capillaries in the extremities back to the heart. Peripheral veins are the most common intravenous access method in both hospitals and paramedic services for a peripheral intravenous (IV) line for intravenous therapy. In some cases blockages in the peripheral arteries may be treated with catheterization and balloon dilatation instead of surgery.
The Heart is more of a Fluid Control Valve that Regulates the Flow of Blood, and not so much a pump. Fluid Mechanics.
Heart May Not Be a Pump: Thomas Cowan on Cardiovascular Disease (youtube) - Thomas Cowan, MD shares compelling evidence that ‘charged water’ drives peripheral circulation and the heart’s job is to actually slow this down. (electrically charged water drives peripheral circulation).
Hemodynamics is the dynamics of blood flow. The circulatory system is controlled by homeostatic mechanisms, such as hydraulic circuits are controlled by control systems. Hemodynamic response continuously monitors and adjusts to conditions in the body and its environment. Thus hemodynamics explains the physical laws that govern the flow of blood in the blood vessels. Cardiac output (v = Q/A) or v = velocity (cm/s) , Q = blood flow (ml/s) , A = cross sectional area (cm2). Blood flow ensures the transportation of nutrients, hormones, metabolic wastes, O2 and CO2 throughout the body to maintain cell-level metabolism, the regulation of the pH, osmotic pressure and temperature of the whole body, and the protection from microbial and mechanical harms.
Myocardial Infarction also known as a Heart Attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest. Most MIs occur due to coronary artery disease. Risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet and excessive alcohol intake, among others. The complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque is usually the underlying mechanism of an MI. MIs are less commonly caused by coronary artery spasms, which may be due to cocaine, significant emotional stress and extreme cold, among others. A number of tests are useful to help with diagnosis, including electrocardiograms (ECGs), blood tests and coronary angiography. An ECG, which is a recording of the heart's electrical activity, may confirm an ST elevation MI (STEMI), if ST elevation is present. Commonly used blood tests include troponin and less often creatine kinase MB. Stress - Emotions.
Symptoms and Warning Signs of a Heart Attack
Heart Attack Quiz
How the Heart Works 3D Video (youtube)
Heart Intelligence (video)
How Low Oxygen Levels in the Heart predispose people to Cardiac Arrhythmias. Research shows that within seconds, at low levels of oxygen (hypoxia), a protein called small ubiquitin-like modifier (SUMO) is linked to the inside of the sodium channels which are responsible for starting each heartbeat. And, while SUMOylated channels open as they should to start the heartbeat, they re-open when they should be closed. The result is abnormal sodium currents that predispose to dangerous cardiac rhythms. Every heartbeat begins when sodium channels open and ions to rush into heart cells -- this starts the action potential that causes the heart muscle to contract. When functioning normally, the sodium channels close quickly after opening and stay closed. Thereafter, potassium channels open, ions leave the heart cells, and the action potential ends in a timely fashion, so the muscle can relax in preparation for the next beat. If sodium channels re-open and produce late sodium currents, as observed in this study with low oxygen levels, the action potential is prolonged and new electrical activity can begin before the heart has recovered risking dangerous, disorganized rhythms. This new research shows how rapid SUMOylation of cell surface cardiac sodium channels causes late sodium current in response to hypoxia, a challenge that confronts many people with heart disease.
Arrhythmogenic Right Ventricular Cardiomyopathy (British Heart Foundation)
New drug for hypertrophic cardiomyopathy reduces heart mass. A medication has impacted heart muscle thickness and function for patients with the most common inherited heart condition, hypertrophic cardiomyopathy, rather than simply addressing their symptoms. The medication works by blocking a protein called myosin from interacting too much with other motor proteins, which then allows the heart muscle to squeeze and relax more normally. Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle becomes abnormally thick (hypertrophied). The thickened heart muscle can make it harder for the heart to pump blood. In HCM, the motor proteins interact with each other too much, causing over-vigorous squeeze of the muscle and causing stiffness of the muscle.
American Heart Association
Hydrogel to Repair Heart. Injectable hydrogel that aims to repair damage and restore cardiac function in heart failure patients who previously suffered a heart attack. VentriGel hydrogel made from the natural scaffolding of cardiac muscle tissue, also known as extracellular matrix, or ECM. There are an estimated 785,000 new heart attack cases in the United States each year, with no established treatment for repairing the resulting damage to cardiac tissue.
Cardiovascular Diseases killed 17.5 million People in 2012
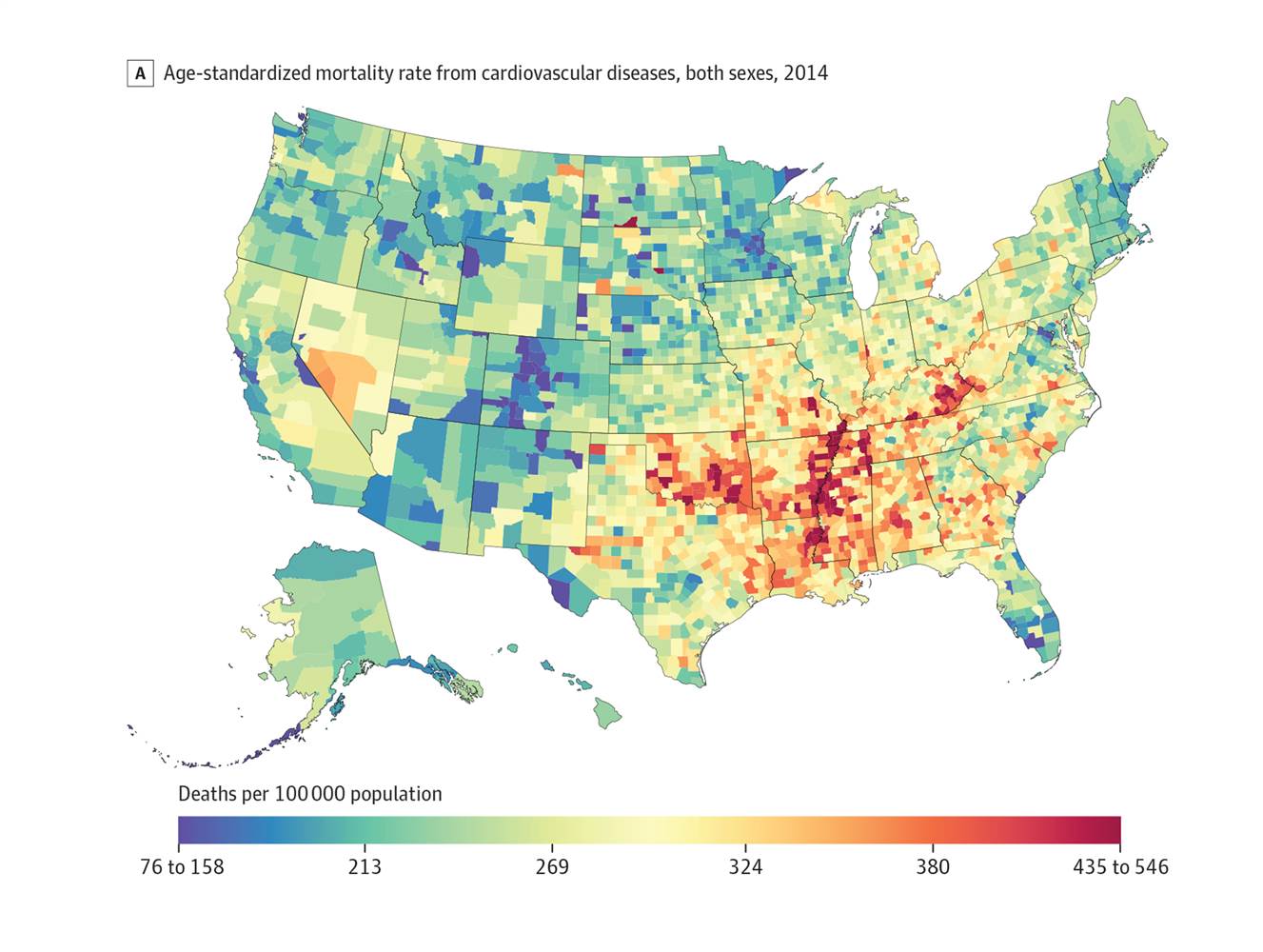 The incidence of
coronary heart disease in the U.S. declined nearly 20 percent from
1983 to 2011, mostly because people are
eating better,
exercising and avoiding
toxins.
The incidence of
coronary heart disease in the U.S. declined nearly 20 percent from
1983 to 2011, mostly because people are
eating better,
exercising and avoiding
toxins.
Unhealthy diets linked to more than 400,000 cardiovascular deaths.
Carotid Artery Stenosis is the narrowing of the blood vessels in the neck that carry blood from the heart to the brain. Carotid artery stenosis can be caused by cholesterol build-up in the blood vessels (atherosclerosis). Blood clots can form in this
area and travel up to the brain. Endothelium.
Dietary supplement shows promise for reversing cardiovascular aging. A novel nutraceutical called nicotinomide riboside has been found to kick-start the same biological pathways as calorie restriction does, and boost arterial health in people with mild hypertension.
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. Others may have shortness of breath, feel tired, or have swelling of the legs due to heart failure. An irregular heart beat may occur as well as fainting. Those affected are at an increased risk of sudden cardiac death.
Heart Disease - Videos (youtube) - Heart Disease Symptoms (webMd)
"I will give you a new heart and put a new spirit in you; I will remove from you your heart of stone and give you a heart of flesh." Ezekiel 36:26 (wiki).
Causes - The Food you Eat can Kill you
Heart Failure Afflicts 5.7 million Americans, Costs the Country $30.7 Billion Every Year.
Scientists create Heart Cells better, faster and stronger. GATA4 is a protein that in humans is encoded by the GATA4 gene. MEF2C also known as MADS box transcription enhancer factor 2, polypeptide C is a protein that in humans is encoded by the MEF2C gene. MEF2C is a transcription factor in the Mef2 family. TBX5 (gene) is a protein that in humans is encoded by the TBX5 gene.
Heart Rate - Pulse
Heart Sounds are the noises generated by the beating heart and the resultant flow of blood through it. Specifically, the sounds reflect the turbulence created when the heart valves snap shut. In cardiac auscultation, an examiner may use a stethoscope to listen for these unique and distinct sounds that provide important auditory data regarding the condition of the heart. Vitals.
Stethoscope is an acoustic medical device for auscultation, or listening to the internal sounds of an animal or human body. It typically has a small disc-shaped resonator that is placed against the chest, and two tubes connected to earpieces. It is often used to listen to lung and heart sounds. It is also used to listen to intestines and blood flow in arteries and veins. In combination with a sphygmomanometer, it is commonly used for measurements of blood pressure. Less commonly, "mechanic's stethoscopes" are used to listen to internal sounds made by machines, such as diagnosing a malfunctioning automobile engine by listening to the sounds of its internal parts. Stethoscopes can also be used to check scientific vacuum chambers for leaks, and for various other small-scale acoustic monitoring tasks. A stethoscope that intensifies auscultatory sounds is called phonendoscope.
Heart Rate is the speed of the heartbeat measured by the number of contractions of the heart per minute (bpm). The heart rate can vary according to the body's physical needs, including the need to absorb oxygen and excrete carbon dioxide. It is usually equal or close to the pulse measured at any peripheral point. Activities that can provoke change include physical exercise, sleep, anxiety, stress, illness, and ingestion of drugs. Breathing.
Heart Rate Variability is the physiological phenomenon of variation in the time interval between heartbeats. It is measured by the variation in the beat-to-beat interval.
When a nerve or muscle cell is at "rest", its membrane potential is called the resting membrane potential. In a typical neuron, this is about –70 millivolts (mV). The minus sign indicates that the inside of the cell is negative with respect to the surrounding extracellular fluid.
Supraventricular Tachycardia is an abnormally fast heart rhythm arising from improper electrical activity in the upper part of the heart. There are four main types: atrial fibrillation, paroxysmal supraventricular tachycardia (PSVT), atrial flutter, and Wolff–Parkinson–White syndrome. Symptoms may include palpitations, feeling faint, sweating, shortness of breath, or chest pain. They start from either the atria or atrioventricular node. They are generally due to one of two mechanisms: re-entry or increased automaticity. The other type of fast heart rhythm is ventricular arrhythmias—rapid rhythms that start within the ventricle. Diagnosis is typically by electrocardiogram (ECG), holter monitor, or event monitor. Blood tests may be done to rule out specific underlying causes such as hyperthyroidism or electrolyte abnormalities.
Tachycardia is the medical term for a heart rate over 100 beats per minute. A fast heart rate.
Bradycardia is a heart rate that's too slow. What's considered too slow can depend on your age and physical condition. Elderly people, for example, are more prone to bradycardia. In general, for adults, a resting heart rate of fewer than 60 beats per minute (BPM) qualifies as bradycardia. Slower-than-expected heart rate, generally beating fewer than 60 beats per minute. Bradycardia can be a serious problem if the heart doesn't pump enough oxygen-rich blood to the body.
Pulse represents the tactile arterial palpation of the heartbeat by trained fingertips.
Normal Resting Heart Rate for adults over the age of 10 years, including older adults, is between 60 and 100 beats per minute (bpm). Highly trained athletes may have a resting heart rate from 60 bpm to 40 beats per minute. The resting heart rate can vary within this normal range. The heart speeds up and slows down to accommodate your changing need for oxygen. What is a "normal" heart rate varies from person to person. However, an unusually high resting heart rate or low maximum heart rate may signify an increased risk of heart attack and death. The rate at which your heart is beating when it is working its hardest to meet your body's oxygen needs is your maximum heart rate. Your maximum heart rate plays a major role in setting your aerobic capacity—the amount of oxygen you are able to consume. A bigger, more powerful heart compensates for a slower speed by moving more blood with each stroke. Some medications—particularly beta blockers—can lower your heart rate. Physical activity and resting pulse rate in older adults: findings from a randomized controlled trial. Elevated resting pulse rate (RPR) is a well-recognized risk factor for adverse outcomes. Generally, a lower heart rate at rest implies more efficient heart function and better cardiovascular fitness.
Athlete's Resting Heart Rate may be considered low when compared to the general population. A young, healthy athlete may have a heart rate of 30 to 40 bpm. This means the heart beats fewer times per minute than it would in a nonathlete. When running, you should train at 50 to 85 percent of your maximum heart rate. If you're 20 years old you should have around 100-170 beats per minute (bpm) as your Target HR Zone of 50-85% when running. Your max heart rate should be 200 bpm. If you're 40 years old, 90-153 bpm on average and 180 bpm maximum. 70 years old, 75-128 bpm and 150 bpm max heart rate.
Athletic Heart Syndrome is a non-pathological condition commonly seen in sports medicine in which the human heart is enlarged, and the resting heart rate is lower than normal. The athlete's heart is associated with physiological remodeling as a consequence of repetitive cardiac loading. Athlete's heart is common in athletes who routinely exercise more than an hour a day, and occurs primarily in endurance athletes, though it can occasionally arise in heavy weight trainers. The condition is generally considered benign, but may occasionally hide a serious medical condition, or may even be mistaken for one.
Electrocardiography is the process of recording the electrical activity of the heart over a period of time using electrodes placed on the skin. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle's electrophysiologic pattern of depolarizing and repolarizing during each heartbeat. It is a very commonly performed cardiology test. In a conventional 12-lead ECG, 10 electrodes are placed on the patient's limbs and on the surface of the chest. The overall magnitude of the heart's electrical potential is then measured from 12 different angles ("leads") and is recorded over a period of time (usually 10 seconds). In this way, the overall magnitude and direction of the heart's electrical depolarization is captured at each moment throughout the cardiac cycle. The graph of voltage versus time produced by this noninvasive medical procedure is referred to as an electrocardiogram. During each heartbeat, a healthy heart has an orderly progression of depolarization that starts with pacemaker cells in the sinoatrial node, spreads out through the atrium, passes through the atrioventricular node down into the bundle of His and into the Purkinje fibers, spreading down and to the left throughout the ventricles. This orderly pattern of depolarization gives rise to the characteristic ECG tracing. To the trained clinician, an ECG conveys a large amount of information about the structure of the heart and the function of its electrical conduction system. Among other things, an ECG can be used to measure the rate and rhythm of heartbeats, the size and position of the heart chambers, the presence of any damage to the heart's muscle cells or conduction system, the effects of cardiac drugs, and the function of implanted pacemakers.
Ventricular Fibrillation is when the heart quivers instead of pumps due to disorganized electrical activity in the ventricles. It results in cardiac arrest with loss of consciousness and no pulse. This is followed by irreversible death without treatment. Ventricular fibrillation is found initially in about 10% of people in cardiac arrest.
Arrhythmia is a problem with the rate or rhythm of your heartbeat. It means that your heart beats too quickly, too slowly, or with an irregular pattern. When the heart beats faster than normal, it is called tachycardia.
Cardiac Arrhythmia Irregular Heartbeat the heartbeat is irregular, too fast, or too slow. A heart rate that is too fast – above 100 beats per minute in adults is called tachycardia and a heart rate that is too slow – below 60 beats per minute – is called bradycardia.
Defibrillation is a treatment for life-threatening cardiac dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing ventricular tachycardia (VT). Defibrillator delivers a dose of electric current (often called a countershock) to the heart.
LED Lamp Automatically Resets Racing Heart with a Bioelectronic Defibrillator that detects fast arrhythmias in the atrium of a rat’s heart and sends a signal to an LED device placed near the heart. “The flash of light from this LED then causes the heart to generate an electric current itself to halt the arrhythmia. This is made possible by using gene therapy to introduce specific light-sensitive proteins into the heart. This restores the heart’s normal rhythm immediately and automatically.
Palpitations is a perceived abnormality of the heartbeat characterized by awareness of heart muscle contractions in the chest: hard beats, fast beats, irregular beats, and/or pauses. Heart Attack.
Murmur are heart sounds produced when blood flows across one of the heart valves that is loud enough to be heard with a stethoscope. Types of murmurs are due to structural defects in the heart itself.
Heart Rate Monitors for Home use
Researchers develop ‘living diode’ using cardiac muscle cells Using cardiac muscle cells and cardiac fibroblasts – cells found in connective heart tissue – researchers at the University of Notre Dame have created a “living diode,” which can be used for cell-based information processing.
Engineers harvest heart's energy to power life-saving devices. Harnessing the heartbeat to charge batteries.
Marfan Syndrome is a genetic disorder of the connective tissue. The degree to which people are affected varies. People with Marfan tend to be tall, and thin, with long arms, legs, fingers and toes. They also typically have flexible joints and scoliosis. The most serious complications involve the heart and aorta with an increased risk of mitral valve prolapse and aortic aneurysm. Other commonly affected areas include the lungs, eyes, bones and the covering of the spinal cord.
The Heart-Brain Connection - PDF - emWave
A new way to Heal Hearts without surgery: Franz Freudenthal (video and interactive text)
Obesity - Diabetes - Patient Records - Broken Heart (feelings)
Valsalva Maneuver is a breathing method that may slow your heart when it's beating too fast. To do it, you breathe out strongly through your mouth while holding your nose tightly closed. or pinching one's nose shut while expelling air out the mouth as if blowing up a balloon. This creates a forceful strain that can trigger your heart to react and go back into normal rhythm. Variations of the maneuver can be used either in medical examination as a test of cardiac function and autonomic nervous control of the heart, or to clear the ears and sinuses (that is, to equalize pressure between them) when ambient pressure changes, as in diving, hyperbaric oxygen therapy, or air travel. A modified version is done by expiring against a closed glottis, which is the opening between the vocal folds or the rima glottidis. The glottis is crucial in producing vowels and voiced consonants.
Vagal Maneuver is an action used to slow down the heart rate by stimulating the vagus nerve. The vagus nerve is the longest nerve of the autonomic nervous system and helps regulate many critical aspects of human physiology, including heart rate, blood pressure, sweating, and digestion. Stimulation of the nerve releases acetylcholine, which slows the pulse. Simple maneuvers may include holding the breath, coughing, and cold water applied to the face. Over-stimulation of the vagus nerve, however, can cause fainting.
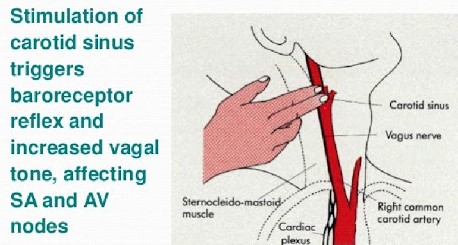 Carotid Sinus Massage is a
simple bedside maneuver that helps to clarify the type and sometimes also
the mechanism of different rhythm disturbances. The major indication for
carotid sinus massage is the dlagnosis of tachyarrhythmias in which the
atrial activity is either absent or intermittently present. This technique
is performed with the patient's neck in an extended position, the head
turned away from the side being massaged. Only one side should be massaged
at a time. Pressure is applied underneath the angle of the jaw in a gentle
circular motion for about 10 seconds.
Carotid Sinus Massage is a
simple bedside maneuver that helps to clarify the type and sometimes also
the mechanism of different rhythm disturbances. The major indication for
carotid sinus massage is the dlagnosis of tachyarrhythmias in which the
atrial activity is either absent or intermittently present. This technique
is performed with the patient's neck in an extended position, the head
turned away from the side being massaged. Only one side should be massaged
at a time. Pressure is applied underneath the angle of the jaw in a gentle
circular motion for about 10 seconds.Carotid Sinus is a dilated area at the base of the internal carotid artery just superior to the bifurcation of the internal carotid and external carotid at the level of the superior border of thyroid cartilage. The carotid sinus extends from the bifurcation to the "true" internal carotid artery. The carotid sinus is sensitive to pressure changes in the arterial blood at this level. It is the major baroreception site in humans and most mammals.
Diving Reflex is triggered specifically by chilling and wetting the nostrils and face while breath-holding, and is sustained via neural processing originating in the carotid chemoreceptors. Or putting your face into a bucket of cold water. The most noticeable effects are on the cardiovascular system, which displays peripheral vasoconstriction, slowed heart rate, redirection of blood to the vital organs to conserve oxygen, release of red blood cells stored in the spleen, and, in humans, heart rhythm irregularities. Although aquatic animals have evolved profound physiological adaptations to conserve oxygen during submersion, the apnea and its duration, bradycardia, vasoconstriction, and redistribution of cardiac output occur also in terrestrial animals as a neural response, but the effects are more profound in natural divers. The diving reflex is also known as the diving response and mammalian diving reflex, is a set of physiological responses to immersion that overrides the basic homeostatic reflexes, and is found in all air-breathing vertebrates studied to date. It optimizes respiration by preferentially distributing oxygen stores to the heart and brain, enabling submersion for an extended time. The diving reflex is exhibited strongly in aquatic mammals, such as seals, otters, dolphins, and muskrats, and exists as a lesser response in other animals, including adult humans, babies up to 6 months old (see infant swimming), and diving birds, such as ducks and penguins.
