BK101
Knowledge Base
First Aid
First Aid is giving emergency care assistance to a person suffering a sudden illness or injury, usually before regular medical aid can be obtained. The key is to preserve life and prevent the condition from worsening, and/or promote recovery. It includes initial intervention in a serious condition prior to professional medical help being available, such as performing CPR while awaiting an ambulance, as well as the complete treatment of minor conditions, such as cuts, hygiene or pain.
Emergency Telephone Number - 9-1-1 - 999

Emergency Medical Services - First Aid Tips - Caregiving
Bites - Burns - Bleeding - Broken Bones - Falling
Chest Pain - Heart Attack - Drug Overdose - CPR
Choking - Poisoning illness - Body Burden
Head - Fever - Eyes - Allergic
Crimes - Police - Fire Safety - Causes of Death
Safetyville USA: Children’s Safety & Health Education Programs.
Apps for First Aid by American Red Cross provides users with clear and concise first aid and CPR instructions to help in the event of an emergency. Emergencies Mobile Apps.
Injury is damage to the body caused by external force. This may be caused by accidents, falls, hits, weapons, and other causes. Major trauma is injury that has the potential to cause prolonged disability or death. In 2013, 4.8 million people died from injuries, up from 4.3 million in 1990. More than 30% of these deaths were transport-related injuries. In 2013, 367,000 children under the age of five died from injuries, down from 766,000 in 1990. Injuries are the cause of 9% of all deaths, and are the sixth-leading cause of death in the world.
Major Trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management and transportation to an appropriate medical facility (called a trauma center) may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment. In 2002, unintentional and intentional injuries were the fifth and seventh leading causes of deaths worldwide, accounting for 6.23% and 2.84% of all deaths. For research purposes the definition often is based on an Injury Severity Score (ISS) of greater than 15.
Physical Therapy - Mental Therapy - Suffering
Invalid is someone who is incapacitated by a chronic illness or injury. A sick person who is confined to home or bed because of illness, disability or injury.
Emergency Essentials Kits
Bug-Out Bag is to survive for seventy-two hours. Survival Kits.
Emergency essentials kits can help you respond to natural disasters or other serious situations. Prepare for the unexpected by putting together a bug out bag of items that could be useful if you needed to evacuate your home. Pack enough to last 24 to 48 hours, and keep your emergency essentials handy. Make sure your family members know where to find the kit. Consider keeping one in your car as well.
Basic Emergency Essentials Kit Includes:
Small, waterproof flashlight or headlamp and extra batteries.
Waterproof matches.
Water, 1 gallon a person a day.
Food that won't spoil, including baby food, if needed.
 Manual can opener for food.
Manual can opener for food.Pet food and supplies, such as a leash, if needed.
Small notepad and waterproof writing instrument.
Blanket.
Cellphone with solar charger.
Battery-powered or hand crank radio and a weather radio with tone alert and extra batteries for both.
Sunscreen.
Insect repellent.
Whistle.
First-aid kit.
Dust mask.
Plastic sheeting and duct tape for improvised shelter.
Wrench or pliers to turn off utilities.
Medicine, a week's supply.
Extra medical supplies or equipment, as needed.
Soap, toothbrush and other personal care items.
Moist towelettes, garbage bags and plastic ties for personal sanitation.
Rescue Equipment
First-Aid Kits
A well-stocked first-aid kit can help you respond effectively to common injuries and emergencies. Keep at least one first-aid kit in your home and one in your car. Store your kits someplace easy to get to and out of the reach of young children. Make sure children old enough to understand the purpose of the kits know where they're stored. You can buy first-aid kits at many drugstores or assemble your own. You may want to tailor your kit based on your activities and needs.
Basic First-Aid Kit Includes:
Adhesive tape.
Elastic wrap bandages.
Bandage strips and "butterfly" bandages in assorted sizes.
Nonstick sterile bandages and roller gauze in assorted sizes.
Eye shield or pad.
Triangular bandage.
Aluminum finger split.
Instant cold packs.
Cotton balls and cotton-tipped swabs.
Disposable nonlatex examination gloves, several pairs.
Duct tape.
Petroleum jelly or other lubricant.
Plastic bags, assorted sizes.
Safety pins in assorted sizes.
Scissors and tweezers.
Soap or hand sanitizer.
Antibiotic ointment.
Antiseptic solution and towelettes.
Eyewash solution.
Thermometer.
Turkey baster or other bulb suction device for flushing wounds.
Breathing barrier.
Syringe, medicine cup or spoon.
First-aid manual.
Medications.
Aloe vera gel.
Calamine lotion.
Anti-diarrhea medication.
Laxative.
Antacids.
Antihistamine, such as diphenhydramine.
Pain relievers, such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and aspirin.
(never give aspirin to children).
Hydrocortisone cream.
Cough and cold medications.
Personal medications that don't need refrigeration.
Auto-injector of epinephrine, if prescribed by your doctor.
Emergency items
Emergency phone numbers, including contact information for your family doctor and pediatrician, local emergency services, emergency road service providers, and the poison help line, which in the United States is 800-222-1222.
Medical consent forms for each family member.
Medical history forms for each family member.
Small, waterproof flashlight or headlamp and extra batteries.
Waterproof matches.
Small notepad and waterproof writing instrument.
Emergency space blanket.
Cell phone with solar charger.
Sunscreen.
Insect repellant.
Whistle.
VSSLS outdoor utility tools and essential outdoor gear and adventure survival kit, without compromising valuable pack space and weight. Survival.
 Bison Paracord Bracelet Interlaced Cobra Weave. When untied it's 9 Feet
Long and takes at least 15 minutes to unwind. Breaking Strength is 550 Lbs. (550 Cord).
Bison Paracord Bracelet Interlaced Cobra Weave. When untied it's 9 Feet
Long and takes at least 15 minutes to unwind. Breaking Strength is 550 Lbs. (550 Cord).
Super Easy Paracord Instructions (youtube)
Warning: Some Paracord Bracelets have 2 or 3 Cords Fused Together so you might have 2 short pieces of rope. Breaking Strength may also vary.
Give your kit a checkup: Check your first-aid kits regularly to be sure the flashlight batteries work and to replace supplies that have expired or been used up. Consider taking a first-aid course through the American Red Cross. Contact your local chapter for information on classes. Prepare children for medical emergencies in age-appropriate ways. The American Red Cross offers a number of helpful resources, including classes designed to help children understand and use first-aid techniques.
Your Personal Emergency Health Information
Emergency health information for you and your family may be needed at a moment's notice. Make sure that key information is up to date, accurate and handy — it may help you get the care you need in a medical emergency. Nowadays, you may find it useful to store this information in an online patient health record and share it with your doctor and emergency contact person. In fact, you may already have access to a patient portal, which is an electronic health information tool offered by many insurance companies, employers and health care institutions. If you have children, it is important to handle their emergency health information similarly. You may not be available to provide needed information in an emergency. Include in your health record, whether online or on paper, the following information:
Your name, age and sex.
Your address.
Your medication names, doses and schedules.
Your medical equipment.
Your chronic medical conditions, such as epilepsy.
Medical consent form.
Aspects of your health history that could be helpful to emergency medical responders, including allergies and immunization record. Phone numbers for professional emergency contacts, such as your family doctor, local emergency services, emergency road service providers, and the regional poison control center. Phone numbers for a personal emergency contact, such as a friend or a family member who you've asked to serve in this role. Power of Attorney.
Online storage: Many people store their personal health information online with the help of an app or a service. This method allows you to access your information anywhere with a computer or a mobile device. Some tools also help you share information with your doctors, family or emergency contact person. The most important thing is to make sure it can be made readily available in an emergency or if you're unconscious. Two options for storing your information online include: Free or subscription-based personal health record. A personal health record (PHR) includes your most important health information. It's like the electronic health record that your doctor may keep for you. But with a PHR, you maintain it and determine who has access to it. Patient portals. Many health care providers, insurance companies and employers offer their clients or staff access to their electronic health record via patient portals. Knowledge Preservation.
Other storage options: Print versions. If you choose to maintain your emergency health information on paper, keep a number of print copies in handy places. For example, put a copy in your purse, vehicle glove box, first aid kit and emergency kit. You could even try making one small enough to fit in your wallet or on an index card. Consider posting the index card on your refrigerator door so emergency personnel can see it quickly if needed. Portable digital device. Put the list on a cell phone, thumb drive or other device that you keep with you.
Emergency Health Information for You and your Family: Medical consent forms for each family member. Phone numbers for professional emergency contacts, such as your family doctor and pediatrician, local emergency services, emergency road service providers, and the regional poison control center. Phone numbers for a personal emergency contact, such as a friend or a family member who you've asked to serve in this role. Copy of insurance cards, Cash or traveler's checks and change, Maps of the area, An extra set of car keys and house keys. Travel Check List.
First Aid Tips
First Aid Index (mayo clinic)
Everyday-First-Aid (red cross)
First Aid Tips (kids health)
Wild Med
Wilderness First Aid
Emergency First Response
Wilderness Schools
Wilderness Medicine Schools
Emergencies (survival tips)
Freedom of the Hills Deck: 52 Playing Cards
Fever
Body temperature over 98.6 F 37 C, hot forehead. Increase fluid intake. Cool cloth. Aspirin. A fever is a rise in body temperature. It's usually a sign of infection. The fever itself is generally harmless and probably helpful. Fevers usually don't need treatment. The average body temperature is 98.6 F (37 C). But normal body temperature can range between 97 (36.1) and 99 (37.2) or more. Your body temperature can vary depending on how active you are or the time of day. Generally, older people have lower body temperatures than younger people.
The following thermometer readings generally indicate a fever:
Rectal, ear or temporal artery temperature of 100.4 (38 C) or higher.
Oral temperature of 100 F (37.8 C) or higher.
Armpit temperature of 99 F (37.2 C) or higher.
Should I treat a fever?
When you or your child is sick, the main goal is to relieve discomfort and promote rest. Treating a fever neither shortens nor particularly prolongs the course of an illness.
Treating fever in a child
Children with relatively high fevers may not look or act particularly sick. Treating a fever depends on the degree of discomfort. If your child is uncomfortable or restless, these home care strategies may help: Encourage your child to drink fluids. Dress your child in lightweight clothing. If your child feels chilled, use a light blanket until the chills end. Give your child acetaminophen (Tylenol, others) or ibuprofen (Advil, Children's Motrin, others) as directed on the label.
Note these precautions: Don't give aspirin to anyone age 18 or younger Don't give ibuprofen to children under 6 months. Don't give acetaminophen to infants under 6 weeks.
Treating fever in an adult: Treat adults with a fever based on how they look and feel. Adults with fevers of 103 F (39.4 C) or higher will generally look and act sick. Use the same home care strategies as listed for children. When to seek medical advice. Get medical help for a fever if Your child is younger than 3 months and has a fever. Your child is age 3 to 6 months and has a temperature up to 102 F (38.9 C) and seems unusually irritable, lethargic or uncomfortable. Your child is age 3 to 6 months and has a temperature higher than 102 F (38.9 C). Your child is age 6 to 24 months and has a temperature above 102 F (38.9 C) that lasts longer than a day but shows no other symptoms. Your child is 2 to 17 years and has a temperature up to 102 F (38.9 C) and seems unusually irritable, lethargic or uncomfortable. Your child is 2 to 17 years and has a temperature above 102 F (38.9 C) that lasts longer than three days or doesn't respond to medication. An adult has a fever that doesn't respond to medication, is consistently 103 F (39.4 C) or higher, or lasts longer than three days.
When to seek emergency care: Seek emergency medical care if your child has a fever after being left in a hot car or other such potentially dangerous situation and shows any of these warning signs: Fever with no sweating. Severe headache. Seizures. Stiff neck. Confusion. Repeated vomiting or diarrhea. Irritability or significant discomfort. Any worrisome, different or unusual symptoms.
How to take a temperature: Always use a digital thermometer to check someone's temperature. Various types are available, including: Digital thermometers, which can be used in the rectum (rectal), mouth (oral) or armpit (axillary), though an armpit reading is the least accurate. Digital ear thermometers (tympanic membrane). Temporal artery thermometer, which measures the temperature of the temporal artery in the forehead. Because of the potential for mercury exposure or ingestion, glass mercury thermometers have been phased out and are no longer recommended. No matter which type of thermometer you use, take these precautions when using it: Read the instructions that came with the thermometer. Clean it before and after each use with rubbing alcohol or soap and lukewarm water. Don't use the same thermometer for both oral and rectal temperatures. Get two and label which is used where. Never leave a child unattended while taking his or her temperature.
Rectal temperature (for infants): Turn on the digital thermometer and dab petroleum jelly or another lubricant on the tip of the thermometer. Lay the child on his or her stomach. Carefully insert the tip 1/2 to 1 inch (1.3 to 2.5 centimeters) into the rectum. Hold the thermometer and child still until the thermometer beep indicates it's done. To avoid injury, don't let go of the thermometer while it's inside the child. Remove the thermometer and read the number.
Oral temperature: Turn on the digital thermometer. Place the thermometer tip under the tongue. Close the mouth around the thermometer for the recommended amount of time or until the thermometer beep indicates it's done. Remove the thermometer and read the number.
Armpit temperature: Turn on the digital thermometer. Place the thermometer under the armpit, making sure it touches skin, not clothing. Hold the thermometer tightly in place until you hear the thermometer beep indicating it's done. Remove the thermometer and read the number.
Ear temperature: Turn on the digital thermometer. Gently place it in the ear, no further than indicated by the instructions that came with the device. Hold the thermometer tightly in place until you hear the thermometer beep indicating it's done. Remove the thermometer and read the number.
Temporal artery temperature: Turn on the thermometer. Gently sweep it across the forehead and read the number.
Conversion Fahrenheit to Celsius
105 Fahrenheit is 40.5 Celsius
104 Fahrenheit is 40.0 Celsius
103 Fahrenheit is 39.4 Celsius
102 Fahrenheit is 38.9 Celsius
101 Fahrenheit is 38.3 Celsius
100 Fahrenheit is 37.7 Celsius
99 Fahrenheit is 37.2 Celsius
98 Fahrenheit is 36.6 Celsius
97 Fahrenheit is 36.1 Celsius
96 Fahrenheit is 35.5 Celsius
Bleeding
If Bleeding heavily put pressure on the wound with whatever is available to stop or slow down the flow of Blood. Keep pressure on the wound until help arrives. Skin - Bones.
How Apply a Tourniquet - Tourniquets
Bleeding Control - PDF - Bleeding Control Kit - Clotting - Hemorrhaging
Stitches: Most wounds that require closure should be stitched, stapled, or closed with skin adhesives or liquid stitches within 6 to 8 hours after the injury. Some wounds that require treatment can be closed as long as 24 hours after the injury.
Suture is a thread of catgut, silk or wire used by surgeons to stitch tissues together.
Surgical Suture is a medical device used to hold body tissues together after an injury or surgery. Application generally involves using a needle with an attached length of thread. A number of different shapes, sizes, and thread materials have been developed over its millennia of history. Surgeons, physicians, dentists, podiatrists, eye doctors, registered nurses and other trained nursing personnel, medics, clinical pharmacists and veterinarians typically engage in suturing. Surgical knots are used to secure the sutures. Suturing Practice kit includes all the essential suture tools in one package to help train and perfect your suturing skills.
Small Cuts: Clean small cuts with soap and clean cold water and cover with clean bandage.
Adhesive Bandage is a small medical dressing used for injuries not serious enough to require a full-size bandage. Band-Aid (wiki)
Squirtable Elastic Surgical Glue Seals Wounds in 60 Seconds - Kirigami-Style Bandages.
Soy Protein/Cellulose Nanofiber Scaffolds Mimicking Skin Extracellular Matrix for Enhanced Wound Healing.
E-Bandage generates electricity, speeds wound healing in Rats.
Water-Resistant Electronic Skin with Self-Healing abilities created. The skin-like material is conductive, transparent, and can repair itself either in air or when submerged in water. NUS scientists have taken inspiration from underwater invertebrates like jellyfish to create an electronic skin with similar functionality.
New Materials could drive Wound Healing by harnessing natural healing methods with new bioinspired material that interacts with surrounding tissues to promote healing.
Fibronectin is a high-molecular weight (~440kDa) glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. Similar to integrins, fibronectin binds extracellular matrix components such as collagen, fibrin, and heparan sulfate proteoglycans (e.g. syndecans). Fibronectin (FN) mediates a wide variety of cellular interactions with the extracellular matrix (ECM) and plays important roles in cell adhesion, migration, growth and differentiation.
Injectable Bandage Created. Injectable hydrogels are promising materials for achieving hemostasis in case of internal injuries and bleeding, as these biomaterials can be introduced into a wound site using minimally invasive approaches. An ideal injectable bandage should solidify after injection in the wound area and promote a natural Clotting cascade. In addition, the injectable bandage should initiate wound healing response after achieving hemostasis. Commonly used thickening agent known as kappa-carrageenan, obtained from seaweed, to design injectable hydrogels. Hydrogels are a 3-D water swollen polymer network, similar to Jell-O, simulating the structure of human tissues. When kappa-carrageenan is mixed with clay-based nanoparticles, injectable gelatin is obtained. The charged characteristics of clay-based nanoparticles provide hemostatic ability to the hydrogels. Specifically, plasma protein and platelets form Blood adsorption on the gel surface and trigger a blood clotting cascade. Injectable bandages can show a prolonged release of therapeutics that can be used to heal the wound.
Mobile bedside Bioprinter can Heal Wounds and allows bi-layered skin that is filled with a patient's own cells to be printed directly into a wound. 3D Printed Body Parts.
Wound is a type of injury which happens relatively quickly in which skin is torn, cut, or punctured (an open wound), or where blunt force trauma causes a contusion (a closed wound). In pathology, it specifically refers to a sharp injury which damages the dermis of the skin.
Minor Cuts and Scrapes: Minor cuts and scrapes usually don't require a trip to the emergency room. These guidelines can help you care for such wounds: Wash your hands. This helps avoid infection. Also put on disposable protective gloves if they're available. Stop the bleeding. Minor cuts and scrapes usually stop bleeding on their own. If not, apply gentle pressure with a sterile bandage or clean cloth and elevate the wound. Clean the wound. Use clear clean water to rinse the wound. Also clean around the wound with soap and a washcloth. Keep soap out of the wound, as it can cause irritation. If dirt or debris remains in the wound after washing, use tweezers cleaned with alcohol to remove the particles. If debris still remains, see your doctor. Thorough cleaning reduces the risk of infection and tetanus. There's no need to use hydrogen peroxide, iodine or an iodine-containing cleanser, which can be irritating to tissue already injured. Apply an antibiotic. Apply a thin layer of an antibiotic cream or ointment (Neosporin, Polysporin) to help keep the surface moist. These products don't make the wound heal faster. But they can discourage infection and help the body's natural healing process. Certain ingredients in some ointments can cause a mild rash in some people. If a rash appears, stop using the ointment. Cover the wound. Bandages can help keep the wound clean and keep harmful bacteria out. If the injury is just a minor scrape, or scratch, leave it uncovered. Change the dressing. Do this at least once a day or whenever the bandage becomes wet or dirty. If the injured person is allergic to the adhesive in tapes and bandages, switch to adhesive-free dressings or sterile gauze held in place with paper tape, rolled gauze or a loosely applied elastic bandage. These supplies generally are available at pharmacies. After the wound has healed enough to make infection unlikely, you can leave it uncovered, as exposure to the air will speed healing. Get stitches for deep wounds. A deep — all the way through the skin — gaping or jagged wound with exposed fat or muscle will need stitches. Adhesive strips or butterfly tape may hold a minor cut together, but if you can't easily close the wound, see your doctor as soon as possible. Proper closure within a few hours minimizes scarring and reduces the risk of infection. Watch for signs of infection. See your doctor if the wound isn't healing or you notice any redness, increasing pain, drainage, warmth or swelling. Get a tetanus shot. If the injured person hasn't had a tetanus shot in the past five years and the wound is deep or dirty, he or she may need a booster shot, as soon as possible. Topical antibiotic triggers unexpected antiviral response. Neomycin, which decreased the herpes virus and symptoms in infected mice.
Antiseptic are antimicrobial substances that are applied to living tissue/skin to reduce the possibility of infection, sepsis, or putrefaction. Antiseptics are generally distinguished from antibiotics by the latter's ability to be transported through the lymphatic system to destroy bacteria within the body, and from disinfectants, which destroy microorganisms found on non-living objects. Some antiseptics are true germicides, capable of destroying microbes (bacteriocidal), while others are bacteriostatic and only prevent or inhibit their growth. Antibacterials are antiseptics that have the proven ability to act against bacteria. Microbicides which destroy virus particles are called viricides or antivirals.
Hydrogen Peroxide is a chemical compound with the formula H2O2. In its pure form, it is a pale blue, clear liquid, slightly more viscous than water. Hydrogen peroxide is the simplest peroxide (a compound with an oxygen–oxygen single bond). It is used as an oxidizer, bleaching agent and antiseptic. Concentrated hydrogen peroxide, or "high-test peroxide", is a reactive oxygen species and has been used as a propellant in rocketry. Its chemistry is dominated by the nature of its unstable peroxide bond. Hydrogen peroxide is unstable and slowly decomposes in the presence of base or a catalyst. Because of its instability, hydrogen peroxide is typically stored with a stabilizer in a weakly acidic solution. Hydrogen peroxide is found in biological systems including the human body. Enzymes that use or decompose hydrogen peroxide are classified as peroxidases.
Puncture Wound: A puncture wound doesn't usually cause excessive bleeding. Often the wound seems to close almost instantly. But this doesn't mean treatment isn't necessary. A puncture wound — such as from stepping on a nail — can be dangerous because of the risk of infection. To take care of a puncture wound: Wash your hands. This helps avoid infection. Stop the bleeding. Apply gentle pressure with a bandage or clean cloth. Clean the wound. Rinse the wound with clear water. If dirt or debris remains in the wound after washing, use tweezers cleaned with alcohol to remove the particles. If debris still remains, see a doctor. Clean the area around the wound with soap and a washcloth. Apply an antibiotic. Apply a thin layer of an antibiotic cream or ointment (Neosporin, Polysporin). Certain ingredients in some ointments can cause a mild rash in some people. If a rash appears, stop using the ointment. Cover the wound. Bandages can help keep the wound clean and keep harmful bacteria out. Change the dressing. Do this at least once a day or whenever the bandage becomes wet or dirty. Watch for signs of infection. See a doctor if the wound isn't healing or you notice any redness, increasing pain, drainage, warmth or swelling.
Get immediate medical help if the wound: Keeps bleeding after a few minutes of direct pressure. Is the result of an animal or human bite Is deep, dirty or caused by a metal object. If the injured person hasn't had a tetanus shot in the past five years and the wound is deep or dirty, your doctor may recommend a booster. The injured person should have the booster shot within 48 hours of the injury. If the wound was caused by a cat or a dog, try to confirm that its rabies vaccination is up to date. If it was caused by a wild animal, seek advice from your doctor about which animals are most likely to carry rabies.
Exsanguination is the loss of blood to a degree sufficient to cause death. Depending upon the age, health, and fitness level of the individual, people can die from losing half to two-thirds of their blood; a loss of roughly one-third of the blood volume is considered very serious. Even a single deep cut can warrant suturing and hospitalization, especially if trauma, a vein or artery, or another comorbidity is involved. The word originates from Latin. (bleed out).
Thorn and other things under the surface of the skin: You can usually safely remove a small foreign object — such as a wood splinter, thorn, fiberglass or glass — that's just under the surface of the skin: Wash your hands and clean the area well with soap and water. Use tweezers cleaned with rubbing alcohol to remove the object. A magnifying glass may help you see better. If the object is under the surface of the skin, sterilize a clean, sharp needle by wiping it with rubbing alcohol. Use the needle to gently lift or break the skin over the object. Lift the tip of the object out and grasp it with your tweezers. Squeeze the wound gently to allow bleeding to wash out germs. Wash the area again and pat dry. Apply an antibiotic ointment. Seek prompt medical help for a foreign object that seems to be more deeply embedded in the skin or muscle. Follow these precautions and steps first: Don't try to remove the object. Doing so could cause further harm. If needed, control bleeding by pressing firmly around the object to bring the edges of the wound together and by raising the injury higher than the heart. Bandage the wound. First put a piece of gauze over the object. Then, if it helps, put clean padding around the object before binding the wound securely with a bandage or a piece of clean cloth. Take care not to press too hard on the object. In addition, seek medical help if: The object doesn't come out easily. The injury involves an eye. The wound is deep or dirty and the injured person's last tetanus shot was more than five years ago. The doctor may recommend a booster shot.
Researchers turn open Wounds into Skin. Technique to directly convert the cells in an open wound into new skin cells. The approach relies on reprogramming the cells to a stem-cell-like state and could be useful for healing wounds and skin damage, countering the effects of aging and helping us to better understand skin cancer.
Groundbreaking new Reusable Adhesive works Underwater. Researchers have introduced a new cutting-edge reusable adhesive that activates in seconds, works underwater, and is strong enough to deadlift 11 pounds: shape memory polymers (SMPs). Dry adhesives, such as those inspired by gecko feet, are believed to be inadequate to achieve high adhesion to a wet or submerged surface. This belief has been nullified because of our SMP reversible dry adhesives.
Dry Glue is an adhesion product based upon the adaptations of geckos' feet that allow them to climb sheer surfaces such as vertical glass. Synthetic equivalents use carbon nanotubes as synthetic setae on reusable adhesive patches.
Shape-Memory Polymer are polymeric smart materials that have the ability to return from a deformed state (temporary shape) to their original (permanent) shape induced by an external stimulus (trigger), such as temperature change.
Smart Polymer are high-performance polymers that change according to the environment they are in. Such materials can be sensitive to a number of factors, such as temperature, humidity, pH, the wavelength or intensity of light or an electrical or magnetic field and can respond in various ways, like altering colour or transparency, becoming conductive or permeable to water or changing shape (shape memory polymers). Usually, slight changes in the environment are sufficient to induce large changes in the polymer's properties. Meta-Materials.
Frostbite: Skin flushed then changing to white or greyish yellow. Blister my appear. Cold and numb. Pain. Do not rub area. Quickly warm by immersing in tepid water 102-105F. If far from warm shelter keep extremity cold during transport.
Animal Bites
If an animal bites you or your child, follow these guidelines: For minor wounds. If the bite barely breaks the skin and there's no danger of rabies, treat it as a minor wound. Wash the wound thoroughly with soap and water. Apply an antibiotic cream to prevent infection and cover the bite with a clean bandage. For deep wounds. If the animal bite creates a deep puncture of the skin or the skin is badly torn and bleeding, apply pressure with a clean, dry cloth to stop the bleeding and see your doctor. For infection. If you notice signs of infection, such as swelling, redness, increased pain or oozing, see your doctor immediately. For suspected rabies. If you suspect the bite was caused by an animal that might carry rabies — including any wild or domestic animal of unknown immunization status, particularly bats — see your doctor immediately. Doctors recommend getting a tetanus shot every 10 years. If your last one was more than five years ago and your wound is deep or dirty, your doctor may recommend a booster. Get the booster as soon as possible after the injury. Domestic pets cause most animal bites. Dogs are more likely to bite than cats. Cat bites, however, are more likely to cause infection because they are usually puncture wounds and can't be thoroughly cleaned. Bites from nonimmunized domestic animals and wild animals carry the risk of rabies. Rabies is more common in bats, raccoons, skunks and foxes than in cats and dogs. Rabbits, squirrels and other rodents rarely carry rabies. The Centers for Disease Control and Prevention recommends that children or adults exposed to bats, or who are sleeping and discover bats present, seek medical advice, even if they don't think they've been bitten. This is because bat bite marks can be hard to see. Seek prompt attention if: The wound is a deep puncture or you're not sure how serious it is. The skin is badly torn and bleeding significantly — first apply pressure with a bandage or clean cloth to stop the bleeding. You notice increasing swelling, redness, pain or oozing, which are warning signs of infection. You have questions about your risk of rabies or about rabies prevention. If the bite was caused by a cat or a dog, try to confirm that its rabies vaccination is up to date. If the bite was caused by a wild animal, seek advice from your doctor about which animals are most likely to carry rabies. Bats often carry rabies. And people have been infected without obvious signs of a bite. This is why the Centers for Disease Control and Prevention recommends that people in contact with bats — or even those who are sleeping and awaken to find a bat in the bedroom — seek medical advice about rabies shots, even if they don't think they've been bitten. You haven't had a tetanus shot in the past five years and the wound is deep or dirty. You may need a booster shot.
Snake Bites: Most North American snakes aren't dangerous to humans. Some exceptions include the rattlesnake, coral snake, water moccasin and copperhead. Their bites can be life-threatening. If you are bitten by a venomous snake, call 911 or your local emergency number immediately, especially if the area changes color, begins to swell or is painful. Many hospitals stock antivenom drugs, which may help you.
If possible, take these steps while waiting for medical help: Remain calm and move beyond the snake's striking distance. Remove jewelry and tight clothing before you start to swell. Position yourself, if possible, so that the bite is at or below the level of your heart. Clean the wound, but don't flush it with water. Cover it with a clean, dry dressing.
Caution: Don't use a tourniquet or apply ice. Don't cut the wound or attempt to remove the venom. Don't drink caffeine or alcohol, which could speed the rate at which your body absorbs venom. Don't try to capture the snake. Try to remember its color and shape so that you can describe it, which will help in your treatment. Venomous snakes in North America. Of the venomous snakes found in North America, all but the coral snake have slit-like eyes and are known as pit vipers. Their heads are triangular, with a depression (pit) midway between the eye and nostril on either side of the head.
Other characteristics are unique to certain venomous snakes: Rattlesnakes rattle by shaking the rings at the end of their tails. Water moccasins' mouths have a white, cottony lining. Coral snakes have red, yellow and black rings along the length of their
bodies.
Envenomation is the process by which venom is injected into some animal by the bite (or sting) of a venomous animal. Many kinds of animals, including mammals (e.g., the northern short-tailed shrew, Blarina brevicauda), reptiles (e.g., the king cobra), spiders (e.g., black widows), and insects (e.g., wasps, honey bees, ants and caterpillars), employ venom for hunting and for self-defense. Most venoms are administered by biting the skin of the victim, but some venoms are applied externally, especially to sensitive tissues such as those that surround the eyes. In some reptiles, such as the Gila monster, venom in the saliva enters prey through bites of grooved teeth, but many animals have specialized organs such as hollow teeth (fangs) and tubular stingers that penetrate the prey's skin after which muscles attached to the attacker's venom reservoir forcibly squirt venom deep within the victim's body tissue. Death may occur as a result of bites or stings.
Antivenom also known as antivenin, venom antiserum and antivenom immunoglobulin, is a medication made from antibodies which is used to treat certain venomous bites and stings. They are only recommended if there is significant toxicity or a high risk of toxicity. The specific antivenom needed depends on the species involved. It is given by injection.
Insect Bites and Stings: pain and redness at site of sting or bite. Possible allergic reactions such as shock or difficulty breathing. Apply cold compresses to bites and stings. Calamine lotion may be soothing. Call Doctor if allergic reactions are present, such as rash, wheezing or trouble breathing. Biotraps Ultimate Mosquito Killer
Tick Bites: Most tick bites cause only minor injury. But some ticks may transmit bacteria that cause illnesses, such as Lyme disease or Rocky Mountain spotted fever. To take care of a tick bite. Remove the tick promptly and carefully. Use tweezers to grasp the tick near its head or mouth and pull gently to remove the whole tick without crushing it. Other methods — such as applying petroleum jelly, fingernail polish, rubbing alcohol or a hot match — aren't recommended. If possible, seal the tick in a container. Put the container in a freezer. Your doctor may want to see the tick if you develop signs or symptoms of illness after a tick bite. Wash your hands with soap and water. Also wash the area around the tick bite.
Call 911 or your local emergency number if you develop: A severe headache, Difficulty breathing, Paralysis, Heart palpitations.
Contact your doctor if you aren't able to completely remove the tick. The longer the tick remains attached to your skin, the greater your risk of getting a disease from it. The rash gets bigger. A small red bump may appear at the site of the tick bite. This is normal. But if it develops into a larger rash, perhaps with a bull's-eye pattern, it may indicate Lyme disease. Also consult your doctor if signs and symptoms disappear because you may still be at risk of the disease. Your risk of contracting a disease from a tick bite depends on where you live or travel to, how much time you spend outside in woody and grassy areas, and how well you protect yourself. You develop flu-like signs and symptoms. Fever, chills, fatigue, body aches and a headache may accompany the rash. You think the bite site is infected. Signs and symptoms include redness or oozing. If possible, bring the tick with you to your doctor's appointment.
Tips to Avoid Ticks
Poison Ivey: Clean every place on your skin with a washcloth and soap that you think came in contact with Poison Ivey, Oak or Sumac. You don't get poison Ivey because you touched the leaves, you get it because you did not thoroughly clean yourself with a washcloth and soap within 2 to 8 hours after contact. Remember that Urushiol is hard to get off your skin, just like grease is, except that Urushiol is not visible like greese, so cleaning Urushiol off your skin is not easy. But if you clean all the possible places with a washcloth and soap, you should be fine, and also be itchy and scratchy free.
Allergic Reactions
Broken Bone Fracture
A fracture is a broken bone. It requires medical attention. If the broken bone is the result of major trauma or injury, call 911 or your local emergency number. Also call for emergency help if: The person is unresponsive, isn't breathing or isn't moving. Begin CPR if there's no breathing or heartbeat. There is heavy bleeding. Even gentle pressure or movement causes pain. The limb or joint appears deformed. The bone has pierced the skin. The extremity of the injured arm or leg, such as a toe or finger, is numb or bluish at the tip. You suspect a bone is broken in the neck, head or back. Don't move the person except if necessary to avoid further injury. Immobilize the injured area. Take these actions immediately while waiting for medical help: Stop any bleeding. Apply pressure to the wound with a sterile bandage, a clean cloth or a clean piece of clothing. Don't try to realign the bone or push a bone that's sticking out back in. If you've been trained in how to splint and professional help isn't readily available, apply a splint to the area above and below the fracture sites. Padding the splints can help reduce discomfort. Apply ice packs to limit swelling and help relieve pain. Don't apply ice directly to the skin. Wrap the ice in a towel, piece of cloth or some other material. Treat for shock. If the person feels faint or is breathing in short, rapid breaths, lay the person down with the head slightly lower than the trunk and, if possible, elevate the legs. Encourage the person to support the injury with their hand, or use a cushion or items of clothing to prevent unnecessary movement. Physical Therapy - Spine Diseases.
Bone Fracture is damage or a break in the bone, but not always severed. A Closed Fracture is when the bone breaks but there is no puncture or open wound in the skin. An open fracture or Compound Fracture is one in which the bone breaks through the skin; it may then recede back into the wound and not be visible through the skin. Treatment often involves resetting the bone in place and immobilizing it in a cast or splint to allow it time to heal. Sometimes, surgery or metal rods may be needed to reset the bone. The natural process of healing a fracture starts when the injured bone and surrounding tissues bleed, forming a fracture hematoma. The blood coagulates to form a blood clot situated between the broken fragments. Within a few days, blood vessels grow into the jelly-like matrix of the blood clot. The new blood vessels bring phagocytes to the area, which gradually remove the non-viable material. The blood vessels also bring fibroblasts in the walls of the vessels and these multiply and produce collagen fibres. In this way the blood clot is replaced by a matrix of collagen. Collagen's rubbery consistency allows bone fragments to move only a small amount unless severe or persistent force is applied. At this stage, some of the fibroblasts begin to lay down bone matrix in the form of collagen monomers. These monomers spontaneously assemble to form the bone matrix, for which bone crystals (calcium hydroxyapatite) are deposited in amongst, in the form of insoluble crystals. This mineralization of the collagen matrix stiffens it and transforms it into bone. In fact, bone is a mineralized collagen matrix; if the mineral is dissolved out of bone, it becomes rubbery. Healing bone callus on average, is sufficiently mineralized to show up on X-ray within 6 weeks in adults and less in children. This initial "woven" bone does not have the strong mechanical properties of mature bone. By a process of remodeling, the woven bone is replaced by mature "lamellar" bone. The whole process may take up to 18 months, but in adults, the strength of the healing bone is usually 80% of normal by 3 months after the injury.
Splint is defined as “a rigid or flexible device that maintains in position a displaced or movable part; also used to keep in place and protect an injured part” or as “a rigid or flexible material used to protect, immobilize, or restrict motion in a part.” Splints can be used for injuries that are not severe enough to immobilize the entire injured structure of the body. For instance, a splint can be used for certain fractures, soft tissue sprains, tendon injuries, or injuries awaiting orthopedic treatment. A splint may be static, not allowing motion, or dynamic, allowing controlled motion. Splints can also be used to relieve pain in damaged joints. Splints are quick and easy to apply and do not require a plastering technique. Splints are often made out of some kind of flexible material and a firm pole-like structure for stability. They often buckle or Velcro together. How to Splint Arm Bone Fracture (wikihow) - How to Splint a Broken Arm (youtube) - Inappropriate Fracture Splints
Dislocation:
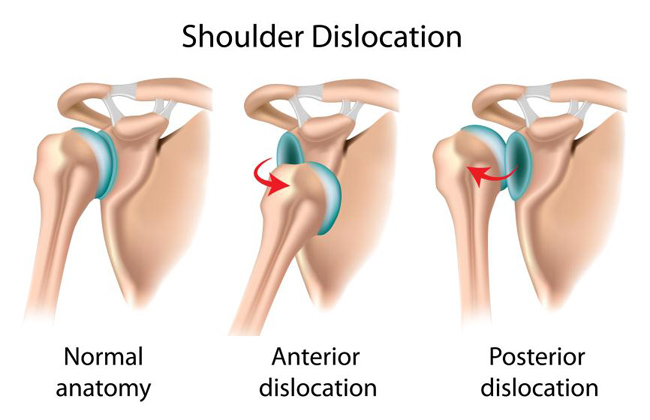 A dislocation is an injury in which the
ends of your bones are forced from their normal positions. The cause
is usually trauma resulting from a fall, an auto accident, or a
collision during contact or high-speed sports. Dislocation usually
involves the body's larger joints. In adults, the most common site of
the injury is the shoulder. In children, it's the elbow. Your thumb and
fingers also are vulnerable if forcibly bent the wrong way. The
injury will temporarily deform and immobilize your joint and may result in
sudden and severe pain and swelling. A dislocation requires prompt
medical attention to return your bones to their proper positions.
If you believe you have dislocated a joint: Don't delay medical care.
Get medical help immediately. Don't move the joint until you receive
help. Splint the affected joint into its fixed position. Don't try to
move a
dislocated joint or force it back into place
unless you know exactly what you're doing. If not done correctly you can damage
the joint and its surrounding muscles, ligaments, nerves or blood
vessels. Treatment for joint dislocation is usually by closed reduction,
that is, skilled
manipulation to return the bones to their normal position.
Reduction should be done only by trained people, because it can cause
injury to soft tissue around the dislocation. Put ice on the injured joint. This can help reduce swelling by
controlling internal bleeding and the buildup of fluids in and around
the injured joint.
A dislocation is an injury in which the
ends of your bones are forced from their normal positions. The cause
is usually trauma resulting from a fall, an auto accident, or a
collision during contact or high-speed sports. Dislocation usually
involves the body's larger joints. In adults, the most common site of
the injury is the shoulder. In children, it's the elbow. Your thumb and
fingers also are vulnerable if forcibly bent the wrong way. The
injury will temporarily deform and immobilize your joint and may result in
sudden and severe pain and swelling. A dislocation requires prompt
medical attention to return your bones to their proper positions.
If you believe you have dislocated a joint: Don't delay medical care.
Get medical help immediately. Don't move the joint until you receive
help. Splint the affected joint into its fixed position. Don't try to
move a
dislocated joint or force it back into place
unless you know exactly what you're doing. If not done correctly you can damage
the joint and its surrounding muscles, ligaments, nerves or blood
vessels. Treatment for joint dislocation is usually by closed reduction,
that is, skilled
manipulation to return the bones to their normal position.
Reduction should be done only by trained people, because it can cause
injury to soft tissue around the dislocation. Put ice on the injured joint. This can help reduce swelling by
controlling internal bleeding and the buildup of fluids in and around
the injured joint. Dislocations Of The Finger - Everything You Need To Know - Dr. Nabil Ebraheim (youtube)
Bone Grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Bone generally has the ability to regenerate completely but requires a very small fracture space or some sort of scaffold to do so. Bone grafts may be autologous (bone harvested from the patient’s own body, often from the iliac crest), allograft (cadaveric bone usually obtained from a bone bank), or synthetic (often made of hydroxyapatite or other naturally occurring and biocompatible substances) with similar mechanical properties to bone. Most bone grafts are expected to be reabsorbed and replaced as the natural bone heals over a few months’ time. The principles involved in successful bone grafts include osteoconduction (guiding the reparative growth of the natural bone), osteoinduction (encouraging undifferentiated cells to become active osteoblasts), and osteogenesis (living bone cells in the graft material contribute to bone remodeling). Osteogenesis only occurs with autograft tissue and allograft cellular bone matrices. Roughly 100,000 broken bones every year in the United States, more than 2 million bone grafts are performed around the world annually in attempts to treat these challenging injuries.
Maxim Bez and colleagues devised a two-step gene therapy method coupled with FDA-approved ultrasound and microbubbles that completely healed nonunion fractures in pigs within eight weeks of treatment. First, researchers placed a collagen scaffold at the site of the break to provide a welcoming niche for bone progenitor cells. Next, they injected microbubbles mixed with genetic material for a bone growth factor. Pulses of sound from an ultrasound wand promoted uptake of the growth factor DNA by progenitor cells, which stimulated bone growth.
Pulsed Electromagnetic Field Therapy uses electromagnetic fields in an attempt to heal non-union fractures and depression. By 2007 the FDA had cleared several such stimulation devices.
A Thermoresponsive Polydiolcitrate-gelatin Scaffold and delivery system mediates effective bone formation from BMP9-transduced mesenchymal stem cells. PPCN-g. New Material Regrows Bone.
Strains and Sprains: Get the person to rest. An ice pack is ice or frozen vegetables wrapped in something such as a tea towel. Applying it to the injury will reduce the swelling and pain. Physical Therapy
Strain is an acute or chronic soft tissue injury that occurs to a muscle, tendon, or both (contractile components). The equivalent injury to a ligament is a sprain.
Sprain is damage to one or more ligaments in a joint, often caused by trauma or the joint being taken beyond its functional range of motion. The severity of sprain ranges from a minor injury which resolves in a few days to a major rupture of one or more ligaments requiring surgical fixation and a period of immobilization. Sprains can occur in any joint but are most common in the ankle and wrist.
Bruise: A bruise forms when a blow breaks blood vessels near your skin's surface, allowing a small amount of blood to leak into the tissues under your skin. The trapped blood may cause a bruise that at first looks like a black-and-blue mark and then changes color as it heals. If your skin isn't broken, you don't need a bandage. But you can enhance bruise healing with these simple techniques: Elevate the injured area. Apply an ice pack wrapped in a towel or a cloth dampened with cold water. Do this for about 10 minutes. Repeat several times a day for a day or two after the injury as needed. Rest the bruised area, if possible. Consider acetaminophen (Tylenol, others) for pain relief, or ibuprofen (Advil, Motrin IB, others) for pain relief and to reduce swelling. Consult your doctor if you: Notice very painful swelling in the bruised area/ Are still experiencing pain three days after a seemingly minor injury. Have frequent, large or painful bruises, particularly if your bruises appear on your trunk, back or face, or seem to develop for no known reasons Have easy bruising and a history of significant bleeding, such as during a surgical procedure. Notice a lump (hematoma) form over the bruise. Are experiencing abnormal bleeding elsewhere, such as from your nose or gums or in urine or stool. Suddenly begin bruising, but have no history of bruising. Have a family history of easy bruising or bleeding. These signs and symptoms may indicate a more serious problem, such as a blood-clotting problem or blood-related disease.
Falling
Falling is the second leading cause of accidental death worldwide and is a major cause of personal injury, especially for the elderly. Falls in older adults are an important class of preventable injuries. Builders, electricians, miners, and painters are occupations with high rates of fall injuries. About 226 million cases of a significant accidental falls occurred in 2015. These resulted in 527,000 deaths. The height at which 50% of children die from a fall is between four and five story heights (around 12 to 15 metres or 40 to 50 feet) above the ground.
Places from where falls occur and activities being undertaken.
Falls — 384 out of 991 total deaths in construction in CY 2016 (38.7%).
Falls from Height in the Construction Industry: A Critical Review of the Scientific Literature.
Occupational Ladder Fall Injuries — United States, 2011.
Falling from High Places. It is estimated that the human body reaches 99% of its low level terminal velocity after falling 573 m (1,880 ft) which takes 13 - 14 sec. This is 188-201 km/h (117 - 125 mph) at normal atmospheric pressure in a random posture, but up to 298 km/h (185 mph) in a head down position. It's not the falling that's fatal, it's the deceleration at the end that kills you, or the impact with the ground. Something like water or concrete does this on a sub-meter distance.
Free Fall is any motion of a body where gravity is the only force acting upon it. In the context of general relativity, where gravitation is reduced to a space-time curvature, a body in free fall has no force acting on it.
If you’re falling from an airplane, you will usually have about 1-3 minutes before impact. Steering yourself to the landing spot. You have the ability to travel horizontally a good distance (up to a couple of miles or three kilometers). To steer yourself to the landing spot. From the arch position face down, you can direct your flight forward by pulling your arms slightly back at the shoulders (so that they are not extended forward as much) and straightening (extending) your legs. You can move backward by extending your arms and bending your knees as though you are trying to touch the back of your head with your heels. Right turns may be accomplished while staying in the arch position by twisting your upper body slightly to the right (dipping your right shoulder), and left turns are performed by dipping the left shoulder.
Use the correct landing technique. Remember to relax your body, keep your knees bent, and fall feet first. Fall forward, rather than backward, and protect your head with your arms in case you bounce. If you are in an arch position, get your body vertical well before you hit the ground so that you don’t get caught in some other position at impact (as a guide, keep in mind that at 1,000 feet, depending on your velocity, you have about 6-10 seconds before impact).
Highest Fall Survived without parachute. Vesna Vulović (Yugoslavia, b. 3 January 1950; d. 23 December 2016) was 23 and working as a Jugoslavenski Aerotransport hostess when she survived a fall from 10,160 m (33,333 ft) over Srbská Kamenice, Czechoslovakia (now Czech Republic), on 26 January 1972. According to the official accident report, an explosion tore the DC-9 she was working aboard to pieces in mid-air. Vulović was the only survivor. She was in hospital for 16 months after emerging from a 27 day coma and having many bones broken.
Centrifuge Study of Pilot Tolerance to Acceleration and the Effects of Acceleration on Pilot Performance
Human responses to aerospace environment related to acceleration, vibration, sound, and noise
Study of impact tolerance through free-fall investigations. Final report
Eyes
If you get a foreign object in your eye: Wash your hands with soap and water. Try to flush the object out of your eye with a gentle stream of clean, warm water. Use an eyecup or a small, clean drinking glass positioned with its rim resting on the bone at the base of your eye socket. Another way to flush a foreign object from your eye is to get into a shower and aim a gentle stream of lukewarm water on your forehead over the affected eye while holding your eyelid open. If you're wearing contact lenses, it's best to remove the lens before or while you're irrigating the surface of the eye with water. Sometimes a foreign body can be embedded on the undersurface of the lens.
To help someone else: Wash your hands with soap and water. Seat the person in a well-lighted area. Gently examine the eye to find the object. Pull the lower lid down and ask the person to look up. Then hold the upper lid while the person looks down. If the object is floating in the tear film on the surface of the eye, try using a medicine dropper filled with clean, warm water to flush it out. Or tilt the head back and irrigate the surface of the eye with clean water from a drinking glass or a gentle stream of tap water.
Caution: Don't try to remove an object that's embedded in the eye. Don't rub the eye. Don't try to remove a large object that appears to be embedded in the eye or is sticking out between the lids.
Get immediate medical help if: You can't remove the object with simple irrigation. The object is embedded in the eye. The person with the object in the eye is experiencing abnormal vision. Pain, redness or the sensation of an object in the eye persists after the object is removed.
Chemical Splashes into your Eye: If a chemical splashes into your eye, take these steps immediately. Flush your eye with water. Use clean, lukewarm tap water for at least 20 minutes. Use whichever of these approaches is quickest: Get into the shower and aim a gentle stream of water on your forehead over your affected eye. Or direct the stream on the bridge of your nose if both eyes are affected. Hold the lids of your affected eye or eyes open. Put your head down and turn it to the side. Then hold the lids of your affected eye open under a gently running faucet. If you have access to a work site eye-rinse station, use it. Young children may do best if they lie down in the bathtub or lean back over a sink. Pour a gentle stream of water on the forehead over the affected eye or on the bridge of the nose to flush both eyes. Wash your hands with soap and water. Thoroughly rinse your hands to be sure no chemical or soap is left on them. Remove contact lenses. If they don't come out during the flush, then take them out.
Caution: Don't rub the eye — this may cause further damage. Don't put anything except water or contact lens saline rinse in the eye. And don't use Eye Drops unless emergency personnel tell you to do so. Seek emergency medical assistance. After following the above steps, seek emergency care by an eye specialist (ophthalmologist) or call 911 or your local emergency number. Take the chemical container or the name of the chemical with you to the emergency provider. If readily available, wear sunglasses to help reduce sensitivity to light.
Eye Scratched: Corneal Abrasion: A corneal abrasion is a superficial scratch on the clear, protective "window" at the front of your eye (cornea). Your cornea can be scratched by contact with dust, dirt, sand, wood shavings, metal particles, contact lenses or even the edge of a piece of paper. Corneal abrasions caused by plant matter (such as a pine needle) usually require special attention as they can cause a delayed inflammation inside the eye (iritis). Signs and symptoms of corneal abrasion include: Pain, A gritty feeling in the eye Tearing, Redness, Sensitivity to the light, Headache. In case of corneal abrasion, seek prompt medical attention. Left untreated, it could become infected and result in a corneal ulcer. Immediate steps you can take for a corneal abrasion are to: Rinse your eye with clean water or a saline solution. You can use an eyecup or a small, clean drinking glass positioned with its rim resting on the bone at the base of your eye socket. If you have quick access to a work site eye-rinse station, use it. Rinsing the eye may wash out a foreign object. Blink several times. This may remove small particles. Pull the upper eyelid over the lower eyelid. This may cause your eye to tear, which may help wash out the particle. Or it may cause the lashes of your lower eyelid to brush away an object from under your upper eyelid. Use the following pointers to avoid making the injury worse: Don't try to remove an object that is embedded in your eyeball or makes it difficult to close your eye. Don't rub your eye after an injury. Don't touch your eyeball with cotton swabs, tweezers or other instruments. If you use contact lenses, don't wear them while your eye is healing. Most corneal abrasions heal in a day or two.
Black Eye: A black eye is caused by bleeding under the skin around the eye. Most injuries that cause a black eye aren't serious. But a black eye may indicate a more serious injury, such as an internal injury to the eye or a fracture of the thin bones around the eye. You may have a skull fracture if you have double vision, bruising around both eyes (raccoon eyes) or bleeding from the nose. To take care of a black eye: Apply a cold compress soon after the injury. Using gentle pressure, place a cold pack or a cloth filled with ice to the area around your eye. Take care not to press on the eye itself. Apply cold as soon as possible after the injury to reduce swelling. Repeat several times a day for a day or two. Look for blood. If you see it in the white or colored parts of the eye, seek urgent care by an eye specialist (ophthalmologist). Seek medical care immediately if you have vision problems (double vision, blurring), severe pain, bruising around both eyes, or bleeding in an eye or from the nose. Apply warm-hot compresses. This may be helpful after a few days when the swelling has stabilized. Repeat several times a day for a day or two.
Head Injury: Ask them to rest and apply something cold to the injury (e.g. frozen vegetables wrapped in a tea towel).Applying something cold to the injury will reduce external swelling and pain. In addition to external swelling, when a person suffers a blow to the head, the brain can be shaken inside the skull. This may result in a more serious head injury (e.g. Concussion), which may make them feel sick or drowsy. Brain Trauma.
Nose: If a foreign object becomes lodged in your nose: Don't probe at the object with a cotton swab or other tool. Don't try to inhale the object by forcefully breathing in. Instead, breathe through your mouth until the object is removed. Blow out of your nose gently to try to free the object, but don't blow hard or repeatedly. If only one nostril is affected, close the opposite nostril by applying gentle pressure and then blow out gently through the affected nostril. Gently remove the object if it's visible and you can easily grasp it with tweezers. Don't try to remove an object that isn't visible or easily grasped. Call for emergency medical assistance or go to your local emergency room if these methods fail.
Nose Bleed: Seat patient, tip head back and squeeze nostrils firmly together for 10 minutes. Apply ice packs to back of neck. Cold compresses to nose may help.
Ear: Foreign Object in the Ear: A foreign object in the Ear can cause pain and hearing loss. Usually you know if an object is stuck in your ear, but small children may not be aware of it. If an object becomes lodged in the ear, follow these steps: Don't probe the ear with a tool. Don't attempt to remove the foreign object by probing with a cotton swab, matchstick or any other tool. To do so risks pushing the object farther into the ear and damaging the fragile structures of the middle ear. Remove the object if possible. If the object is clearly visible, pliable and can be grasped easily with tweezers, gently remove it. Try using gravity. Tilt the head to the affected side to try to dislodge the object. Try using oil for an insect. If the foreign object is an insect, tilt the person's head so that the ear with the offending insect is upward. Try to float the insect out by pouring mineral oil, olive oil or baby oil into the ear. The oil should be warm but not hot. As you pour the oil, you can ease the entry of the oil by straightening the ear canal. Pull the earlobe gently backward and upward for an adult, backward and downward for a child. The insect should suffocate and float out in the oil bath. Don't use oil to remove any object other than an insect. Don't use this method for a child if ear tubes are in place or if you think the eardrum may be perforated. Signs of this are pain, bleeding or discharge from the ear. Try washing the object out. Use a bulb ear syringe and warm water to irrigate the object out of the canal, again provided no ear tubes are in place and you don't suspect the eardrum is perforated. If these methods fail or the person continues to experience pain in the ear, reduced hearing or a sensation of something lodged in the ear, seek medical assistance.
Stroke
Strokes are caused by a blockage of the blood supply to the brain. Part of the brain becomes damaged, and this can affect people’s appearance, bodily functions, speech and sight. Think F.A.S.T. Face: is there weakness on one side of their face? Arms: can they raise both arms? Speech: is their speech easily understood? Time: to call 999. Cover person with light blanket. Turn to side if vomiting. Give no stimulants, food or drink. Call Ambulance 911. Some people who might be more susceptible to strokes might have a medical alert device that can alert the appropriate authorities when it detects a medical issue. There are many medical alert devices on the market, but Consumers Advocate has several reviews that can help narrow the choices down
Heart Attack
This pain is caused by a blockage of the blood supply to the heart muscle, and the pain will not ease with rest. The person may have persistent, vice-like chest pain, which may spread to their arms, neck, jaw, back or stomach. A heart attack occurs when an artery that supplies oxygen to your heart muscle becomes blocked. A heart attack may cause chest pain that lasts 15 minutes or longer, or it can also be silent and produce no signs or symptoms. Many people who experience a heart attack have warning signs hours, days or weeks in advance. The earliest warning sign of an attack may be ongoing episodes of chest pain that start when you're physically active and are relieved by rest. Someone having a heart attack may experience none, any or all of the following: Uncomfortable pressure, fullness or squeezing pain in the center of the chest lasting more than a few minutes. Pain spreading to the shoulders, neck, jaw or arms. Lightheadedness, fainting, sweating, nausea or shortness of breath. If you or someone else may be having a heart attack: Call 911 or emergency medical assistance. Don't tough out the symptoms of a heart attack for more than five minutes. If you don't have access to emergency medical services, have a neighbor or friend drive you to the nearest hospital. Drive yourself only as a last resort, and realize that driving yourself puts you and others at risk if your condition suddenly worsens. Chew a regular-strength aspirin. Aspirin reduces blood clotting, which can help blood flow through a narrowed artery that's caused a heart attack. However, don't take aspirin if you are allergic to aspirin, have bleeding problems or take another blood-thinning medication, or if your doctor previously told you not to do so. Take nitroglycerin, if prescribed. If you think you're having a heart attack and your doctor has previously prescribed nitroglycerin for you, take it as directed. Don't take anyone else's nitroglycerin. Begin CPR on the person having a heart attack, if directed. If the person suspected of having a heart attack is unconscious, a 911 dispatcher or another emergency medical specialist may advise you to begin cardiopulmonary resuscitation (CPR). If you haven't received CPR training, doctors recommend skipping mouth-to-mouth rescue breathing and performing only chest compressions (about 100 a minute). The dispatcher can instruct you in the proper procedures until help arrives. If an automated external defibrillator (AED) is available and the person's unconscious, begin CPR while the device is retrieved and set up. Attach the device and follow instructions that will be provided by the AED after it has evaluated the person's condition. CPR Training - Injectable gel helps heart muscle regenerate after heart attack.
Brugada Syndrome is a genetically inherited condition that is characterized by abnormal electrocardiogram (ECG) findings and an increased risk of sudden cardiac death.
Cardiac Arrest is a sudden stop in effective blood flow due to the failure of the heart to contract effectively. Symptoms include loss of consciousness and abnormal or absent breathing. Some people may have chest pain, shortness of breath, or nausea before this occurs. If not treated within minutes, death usually occurs.
Electrocardiography is the process of recording the electrical activity of the heart over a period of time using electrodes placed on the skin. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle's electrophysiologic pattern of depolarizing and repolarizing during each heartbeat. It is a very commonly performed cardiology test.
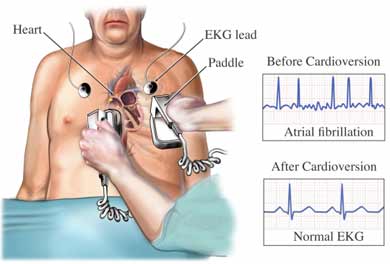 Cardioversion is a medical procedure by which an abnormally fast heart
rate (tachycardia) or other cardiac arrhythmia is converted to a normal
rhythm using electricity or drugs. Synchronized electrical cardioversion
uses a therapeutic dose of electric current to the heart at a specific
moment in the cardiac cycle, restoring the activity of the electrical
conduction system of the heart. (Defibrillation uses a therapeutic dose of
electric current to the heart at a random moment in the cardiac cycle, and
is the most effective resuscitation measure for cardiac arrest associated
with ventricular fibrillation and pulseless ventricular tachycardia.
Pharmacologic cardioversion, also called chemical cardioversion, uses
antiarrhythmia medication instead of an electrical shock.
Cardioversion is a medical procedure by which an abnormally fast heart
rate (tachycardia) or other cardiac arrhythmia is converted to a normal
rhythm using electricity or drugs. Synchronized electrical cardioversion
uses a therapeutic dose of electric current to the heart at a specific
moment in the cardiac cycle, restoring the activity of the electrical
conduction system of the heart. (Defibrillation uses a therapeutic dose of
electric current to the heart at a random moment in the cardiac cycle, and
is the most effective resuscitation measure for cardiac arrest associated
with ventricular fibrillation and pulseless ventricular tachycardia.
Pharmacologic cardioversion, also called chemical cardioversion, uses
antiarrhythmia medication instead of an electrical shock.
Automated External Defibrillator is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation and ventricular tachycardia in a patient, and is able to treat them through defibrillation, the application of electrical therapy which stops the arrhythmia, allowing the heart to reestablish an effective rhythm. With simple audio and visual commands, AEDs are designed to be simple to use for the layperson, and the use of AEDs is taught in many first aid, certified first responder, and basic life support (BLS) level Cardiopulmonary Resuscitation (CPR) classes.
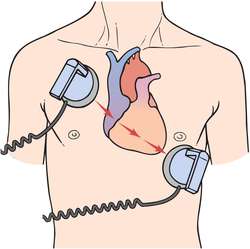 Defibrillation is a treatment for life-threatening cardiac
dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing
ventricular tachycardia (VT). A defibrillator delivers a dose of electric
current (often called a countershock) to the heart. Although not fully
understood, this would depolarize a large amount of the heart muscle,
ending the dysrhythmia. Subsequently, the body's natural pacemaker in the
sinoatrial node of the heart is able to re-establish normal sinus rhythm.
Defibrillation is a treatment for life-threatening cardiac
dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing
ventricular tachycardia (VT). A defibrillator delivers a dose of electric
current (often called a countershock) to the heart. Although not fully
understood, this would depolarize a large amount of the heart muscle,
ending the dysrhythmia. Subsequently, the body's natural pacemaker in the
sinoatrial node of the heart is able to re-establish normal sinus rhythm.
Heart-Muscle Patches made with Human Cells improve Heart Attack Recovery.
Chest Pain: Causes of chest pain can vary from minor problems, such as indigestion or stress, to serious medical emergencies, such as a heart attack or pulmonary embolism. The specific cause of chest pain can be difficult to interpret. Finding the cause of your chest pain can be challenging, especially if you've never had prior symptoms. Even doctors may have a difficult time deciding if chest pain is a sign of a heart attack or something less serious, such as indigestion. If you have unexplained chest pain lasting more than a few minutes, it is better to seek emergency medical assistance than to try and diagnose the cause yourself. As with other sudden, unexplained pains, chest pain may be a signal for you to get medical help. Use the following information to help determine whether your chest pain is a medical emergency.
Angina: Angina is chest pain or discomfort caused by reduced blood flow to your heart muscle. Typically the term "angina" is used when you've already been given the diagnosis of heart disease related to atherosclerosis. Angina may be stable or unstable: Stable angina — persistent, recurring chest pain that usually occurs with exertion and is relatively predictable. Unstable angina — sudden, new chest pain, or a change in the pattern of previously stable angina, that may signal an impending heart attack. Angina is relatively common, but can be hard to distinguish from other types of chest pain, such as the pain or discomfort of indigestion. If you are having angina with any of the following signs and symptoms, it may indicate a more serious condition, such as a heart attack: Pain in your arms, neck, jaw, shoulder or back accompanying chest pain. Nausea. Fatigue. Shortness of breath. Anxiety. Sweating. Dizziness. The severity, duration and type of angina can vary. If you have new or changing chest pain, these new or different symptoms may signal a more dangerous form of angina (unstable angina) or a heart attack. If your angina gets worse or changes, seek medical attention immediately.
Pulmonary embolism: Pulmonary embolism occurs when a clot — usually from the veins of your leg or pelvis — lodges in a pulmonary artery of your lung. The lung tissue served by the artery doesn't get enough blood flow, causing tissue death. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Signs and symptoms of pulmonary embolism may include: Sudden, sharp chest pain often accompanied by shortness of breath. Sudden, unexplained shortness of breath, even without pain. Cough that may produce blood-streaked sputum. Rapid heartbeat associated with shortness of breath. Fainting. Severe anxiety. Unexplained sweating. Pulmonary embolism can be life-threatening. As with a suspected heart attack, call 911 or emergency medical assistance immediately.
Aortic dissection: An aortic dissection is a serious condition in which a tear develops in the inner layer of the aorta, the large blood vessel branching off the heart. Blood surges through this tear into the middle layer of the aorta, causing the inner and middle layers to separate (dissect). If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is usually fatal.
Typical signs and symptoms include: Sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation, that radiates to the neck or down the back. Loss of consciousness (fainting). Shortness of breath. Sudden difficulty speaking, loss of vision, weakness, or paralysis of one side of your body, such as having a stroke. Sweating. Weak pulse in one arm compared with the other. If you are experiencing any of these signs or symptoms, they could be caused by an aortic dissection or some other serious condition. Seek emergency medical assistance immediately.
Pneumonia with pleurisy: Frequent signs and symptoms of pneumonia are chest pain accompanied by chills, fever and a cough that may produce bloody or foul-smelling sputum. When pneumonia occurs with an inflammation of the membranes that surround the lung (pleura), you may have considerable chest discomfort when taking a breath or coughing. This condition is called pleurisy. One sign of pleurisy is that the pain is usually relieved temporarily by holding your breath or putting pressure on the painful area of your chest. This isn't usually true of a heart attack. If you've recently been diagnosed with pneumonia and then start having symptoms of pleurisy, contact your doctor or seek immediate medical attention to determine the cause of your chest pain. Pleurisy alone isn't a medical emergency, but you shouldn't try to make the diagnosis yourself.
Chest wall pain: One of the most common varieties of harmless chest pain is chest wall pain. One kind of chest wall pain is costochondritis. It causes pain and tenderness in and around the cartilage that connects your ribs to your breastbone (sternum). In costochondritis, pressing on a few points along the edge of your sternum often results in considerable tenderness in those small areas. If the pressure of a finger causes similar chest pain, it's unlikely that a serious condition, such as a heart attack, is the cause of your chest pain.
Other causes of chest pain include: Strained chest muscles from overuse or excessive coughing. Chest muscle bruising from minor injury. Short-term, sudden anxiety with rapid breathing. Peptic ulcer disease. Pain from the digestive tract, such as esophageal reflux, peptic ulcer pain or gallbladder pain that may feel similar to heart attack symptoms.
Pericarditis is inflammation of the pericardium (the fibrous sac surrounding the heart). Symptoms typically include sudden onset of sharp chest pain. The pain may also be felt in the shoulders, neck, or back. It is typically better sitting up and worse with lying down or breathing deep. Other symptoms may include fever, weakness, palpitations, and shortness of breath. Occasionally onset of symptoms is gradual.
Reviving cells after a heart attack. Researchers have unraveled potential mechanisms behind the healing power of extracellular vesicles and demonstrated their capacity to not only revive cells after a heart attack but keep cells functioning while deprived of oxygen during a heart attack. The researchers demonstrated this functionality in human tissue using a heart-on-a-chip with embedded sensors that continuously tracked the contractions of the tissue. Extracellular vesicles (EVs) -- nanometer sized messengers that travel between cells to deliver cues and cargo.
Stomach - Belly - Abdominal Pain
Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.
Abdominal Pain is a symptom associated with both non-serious and serious medical issues. Common causes of pain in the abdomen include gastroenteritis and irritable bowel syndrome. About 10% of people have a more serious underlying condition such as appendicitis, leaking or ruptured abdominal aortic aneurysm, diverticulitis, or ectopic pregnancy. In a third of cases the exact cause is unclear. Given that a variety of diseases can cause some form of abdominal pain, a systematic approach to examination of a person and the formulation of a differential diagnosis remains important.
Hernia is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. Hernias come in a number of different types. Inguinal Hernia is a protrusion of abdominal-cavity contents through the inguinal canal. Hiatal Hernia is a type of hernia in which abdominal organs (typically the stomach) slip through the diaphragm into the middle compartment of the chest. If you have a hiatal hernia, part of your stomach comes up through your diaphragm in the hiatal opening. Hiatal hernias are caused by weakened muscle tissues, which can be a result of an especially large hiatus (muscle space), injury, or persistent pressure on surrounding muscles.
Phrenic Nerve is a nerve that originates in the neck (C3-C5) and passes down between the lung and heart to reach the diaphragm. It is important for breathing, as it passes motor information to the diaphragm and receives sensory information from it. There are two phrenic nerves, a left and a right one. The phrenic nerve originates mainly from the 4th cervical nerve, but also receives contributions from the 5th and 3rd cervical nerves (C3-C5) in humans. Thus, the phrenic nerve receives innervation from parts of both the cervical plexus and the brachial plexus of nerves. The phrenic nerves contain motor, sensory, and sympathetic nerve fibers. These nerves provide the only motor supply to the diaphragm as well as sensation to the central tendon. In the thorax, each phrenic nerve supplies the mediastinal pleura and pericardium. The phrenic nerve controls the muscle of the diaphragm. It sends signals to your brain, which allows you to breathe without thinking. If your phrenic nerve becomes irritated or damaged, you may lose the ability to take automatic breaths.
Diaphragm is a sheet of internal skeletal muscle in humans and other mammals that extends across the bottom of the thoracic cavity. The diaphragm separates the thoracic cavity, containing the heart and lungs, from the abdominal cavity and performs an important function in respiration: as the diaphragm contracts, the volume of the thoracic cavity increases and air is drawn into the lungs. Your diaphragm can become temporarily paralyzed if you’ve “had the wind knocked out of you” from a direct hit to your abdomen. Right after the hit, you may have difficulty breathing, as your diaphragm might struggle to fully expand and contract. Other symptoms of temporary paralysis include: hiccups, tightness in the chest, pain in the chest, pain in the stomach. Diaphragm flutter is a rare condition that can be misdiagnosed as a spasm. A diaphragm flutter can also be caused by phrenic nerve irritation. Other symptoms associated with diaphragm flutter include: chest tightness, difficulty breathing, a feeling of pulses in the abdominal wall.
Side Stitches, or cramping in the ribcage, sometimes occur when you first begin exercise training or when that training becomes more intense. For some people, drinking juice or eating right before a workout can increase the possibility of side stiches. To help Raise the arm corresponding to the side of the pain and place that hand on the back of your head. Hold it for 30 to 60 seconds to allow knots to loosen. You can even continue exercising while holding the stretch.
Choking - Can't Breathe - Not Breathing
Swallowing of Foreign Bodies: Dangerous when in air passages. Violently choking and coughing. Bluish facial discoloration. Breathing may stop. If Victim cannot dislodge object. Administer airways obstruction procedure. Hit on back and hold children upside down. Choking occurs when a foreign object becomes lodged in the throat or windpipe, blocking the flow of air. In adults, a piece of food often is the culprit. Young children often swallow small objects. Because choking cuts off oxygen to the brain, administer first aid as quickly as possible. The universal sign for choking is hands clutched to the throat. If the person doesn't give the signal, look for these indications: Inability to talk. Difficulty breathing or noisy breathing. Inability to cough forcefully. Skin, lips and nails turning blue or dusky. Loss of consciousness.
Image (choking) The Heimlich Maneuver (youtube)
If choking is occurring, the Red Cross recommends a "five-and-five" approach to delivering first aid: Give 5 back blows. First, deliver five back blows between the person's shoulder blades with the heel of your hand. Give 5 abdominal thrusts. Perform five abdominal thrusts (also known as the Heimlich maneuver). Alternate between 5 blows and 5 thrusts until the blockage is dislodged. The American Heart Association doesn't teach the back blow technique, only the abdominal thrust procedures. It's OK not to use back blows, if you haven't learned the technique. Both approaches are acceptable.
To perform abdominal thrusts (Heimlich maneuver) on someone else: Stand behind the person. Wrap your arms around the waist. Tip the person forward slightly. Make a fist with one hand. Position it slightly above the person's navel. Grasp the fist with the other hand. Press hard into the abdomen with a quick, upward thrust — as if trying to lift the person up. Perform a total of 5 abdominal thrusts, if needed. If the blockage still isn't dislodged, repeat the five-and-five cycle. If you're the only rescuer, perform back blows and abdominal thrusts before calling 911 or your local emergency number for help. If another person is available, have that person call for help while you perform first aid. If the person becomes unconscious, perform standard CPR with chest compressions and rescue breaths.
To perform abdominal thrusts (Heimlich maneuver) on yourself: First, if you're alone and choking, call 911 or your local emergency number immediately. Then, although you'll be unable to effectively deliver back blows to yourself, you can still perform abdominal thrusts to dislodge the item. Place a fist slightly above your navel. Grasp your fist with the other hand and bend over a hard surface — a countertop or chair will do. Shove your fist inward and upward.
To clear the airway of a pregnant woman or obese person: Position your hands a little bit higher than with a normal Heimlich maneuver, at the base of the breastbone, just above the joining of the lowest ribs. Proceed as with the Heimlich maneuver, pressing hard into the chest, with a quick thrust. Repeat until the food or other blockage is dislodged or the person becomes unconscious.
To clear the airway of an unconscious person: Lower the person on his or her back onto the floor. Clear the airway. If a blockage is visible at the back of the throat or high in the throat, reach a finger into the mouth and sweep out the cause of the blockage. Be careful not to push the food or object deeper into the airway, which can happen easily in young children. Begin cardiopulmonary resuscitation (CPR) if the object remains lodged and the person doesn't respond after you take the above measures. The chest compressions used in CPR may dislodge the object. Remember to recheck the mouth periodically.
To clear the airway of a choking infant younger than age 1: Assume a seated position and hold the infant facedown on your forearm, which is resting on your thigh. Thump the infant gently but firmly five times on the middle of the back using the heel of your hand. The combination of gravity and the back blows should release the blocking object. Hold the infant faceup on your forearm with the head lower than the trunk if the above doesn't work. Using two fingers placed at the center of the infant's breastbone, give five quick chest compressions. Repeat the back blows and chest thrusts if breathing doesn't resume. Call for emergency medical help. Begin infant CPR if one of these techniques opens the airway but the infant doesn't resume breathing. If the child is older than age 1, give abdominal thrusts only. To prepare yourself for these situations, learn the Heimlich maneuver and CPR in a certified first-aid training course.
Swallowed a Foreign Object: If you swallow a foreign object, it will usually pass through your digestive system uneventfully. But some objects can lodge in your esophagus, the tube that connects your throat and stomach. If an object is stuck in your esophagus, you may need to have it removed, especially if it is: A pointed object, which should be removed as quickly as possible to avoid further injury to the esophageal lining. A tiny watch- or calculator-type button battery, which can rapidly cause nearby tissue injury and should be removed from the esophagus without delay, If a person who has swallowed an object is coughing forcefully, encourage him or her to continue coughing and do not interfere. If a swallowed object blocks the airway and the person's condition worsens — the cough becomes silent or breathing becomes more difficult — the American Red Cross recommends the five-and-five approach to first aid: Give 5 back blows. First, deliver five back blows between the person's shoulder blades with the heel of your hand. Give 5 abdominal thrusts. Perform five abdominal thrusts (also known as the Heimlich maneuver).
Abdominal thrusts may injure infants. Use chest compressions instead. Alternate between 5 back blows and 5 abdominal thrusts until the blockage is dislodged. If you're the only rescuer, perform back blows and abdominal thrusts before calling 911 or your local emergency number for help. If another person is available, have that person call for help while you perform first aid. If the person becomes unconscious, help him or her to the ground and begin CPR. After attempted rescue breaths, check the mouth for an object and if visible remove it. Do not perform a blind finger sweep because this could push an object farther into the airway. The American Heart Association does not teach the back-blow technique, only the abdominal thrust procedures. It's OK not to use back blows if you have not learned the back-blow technique. Both approaches are acceptable.
To perform the Heimlich maneuver on someone else: Stand behind the person. Wrap your arms around the waist. Tip the person forward slightly. Make a fist with 1 hand. Position it slightly above the person's navel. Grasp the fist with the other hand. Press hard into the abdomen with a quick, upward thrust — as if trying to lift the person up. Perform a total of 5 abdominal thrusts, if needed. If the blockage still isn't dislodged, repeat the five-and-five cycle. A modified version of the technique is sometimes taught for use with pregnant or obese people. The rescuer places his or her hand in the center of the chest to compress, rather than in the abdomen.
To perform the Heimlich maneuver on yourself: If you're choking and alone, call 911 or your local emergency number immediately. You can't perform back blows on yourself. But you can perform abdominal thrusts. Place a fist slightly above your navel. Grasp your fist with the other hand and bend over a hard surface — a countertop or chair will do. Shove your fist inward and upward.
Inhaled Foreign Object: If you or your child inhales a foreign object, see your doctor. If an inhaled foreign object causes choking, the American Red Cross recommends the "five-and-five" approach to delivering first aid: Give 5 back blows. First, deliver five back blows between the choking person's shoulder blades with the heel of your hand. Give 5 abdominal thrusts. Perform five abdominal thrusts (also known as the Heimlich maneuver). Alternate between 5 blows and 5 thrusts until the blockage is dislodged. If you're the only rescuer, perform back blows and abdominal thrusts before calling 911 or your local emergency number for help. If another person is available, have that person call for help while you perform first aid. The American Heart Association does not teach the back-blow technique, only the abdominal thrust procedures. It's OK not to use back blows if you have not learned the back-blow technique. Both approaches are acceptable.
To perform the Heimlich maneuver on someone else: Stand behind the person. Wrap your arms around the waist. Tip the person forward slightly. Make a fist with 1 hand. Position it slightly above the person's navel. Grasp the fist with the other hand. Press hard into the abdomen with a quick, upward thrust — as if trying to lift the person up. Perform a total of 5 abdominal thrusts, if needed. If the blockage still isn't dislodged, repeat the five-and-five cycle. A modified version of the technique is sometimes taught for use with pregnant or obese people. The rescuer places his or her hand in the center of the chest to compress, rather than in the abdomen.
To perform the Heimlich maneuver on yourself: If you're alone and choking, call 911 or your local emergency number immediately. Then, although you'll be unable to effectively deliver back blows to yourself, you can still perform abdominal thrusts to dislodge the item. Place a fist slightly above your navel. Grasp your fist with the other hand and bend over a hard surface — a countertop or chair. Shove your fist inward and upward
Unresponsive and Breathing: Check breathing by tilting their head backwards and looking and feeling for breaths. When a person is unresponsive their muscles relax and their tongue can block their airway so they can no longer breathe. Tilting their head back opens the airway by pulling the tongue forward. Looking at their chest to see if it’s moving, and feeling for breaths on your cheek, will help you tell if they’re breathing or not. Find out what to do if they are not breathing.
Croup is a disease of infants and young children; harsh coughing and hoarseness and fever and difficult breathing.
Croup (wiki)
CPR - Cardio-Pulmonary Resuscitation
Unresponsive and Not Breathing: Chest compressions help blood continue pumping around the body. This keeps vital organs, including the brain, alive. Many people call this CPR, which stands for Cardio-Pulmonary Resuscitation.
CPR Info-Graph (image) - Infant CPR for babies or very young children.
First Aid & CPR Certification
CPR Training Schools
American CPR
SafeNow CPR Infant CPR
CPR Class
CPR Ed Course
Training for first Responders
Wilderness Medicine School
Wilderness First Responder Training - Videos
Outdoor Safety Courses
Redcross
The Heimlich Maneuver - Heart Attack
Emergency Services - Emergency Personal
EMT or Emergency Medical Technician, is a Health Care Provider of emergency medical services. EMTs are clinicians, trained to respond quickly to emergency situations regarding medical issues, traumatic injuries and accident scenes. Under the British system and those that are influenced by it, they are referred to as ambulance technicians (often shortened to techs), while in the American system and its influenced countries, they are referred to as emergency medical technicians.
Duty of Care - Search and Rescue - Hospitals
Paramedic is a healthcare professional, predominantly in the pre-hospital and out-of-hospital environment, and working mainly as part of emergency medical services (EMS), such as on an ambulance. The scope of practice of a paramedic will vary between countries, but generally includes autonomous decision making around the emergency care of patients. In some countries 'Paramedic' is a protected title and accountable to a professional regulatory body.
First Responder is a person with specialized training who is among the first to arrive and provide assistance at the scene of an emergency, such as an accident, natural disaster, or terrorist attack. First responders typically include paramedics, emergency medical technicians, police officers, firefighters, rescuers, and other trained members of organizations connected with this type of work. A certified first responder is one who has received certification to provide pre-hospital care in a certain jurisdiction, for example, the Certified First Responder in France. A community first responder is a person dispatched to attend medical emergencies until an ambulance arrives. A wilderness first responder is trained to provide pre-hospital care in remote settings and will therefore have skills in ad hoc patient packaging and transport by non-motorized means.
Ambulance is a vehicle for transportation of sick or injured people to, from or between places of treatment for an illness or injury, and in some instances will also provide out of hospital medical care to the patient. The word is often associated with road going emergency ambulances which form part of an emergency medical service, administering emergency care to those with acute medical problems.
Air Medical Services is a comprehensive term covering the use of air transportation, airplane or helicopter, to move patients to and from healthcare facilities and accident scenes. Personnel provide comprehensive prehospital and emergency and critical care to all types of patients during aeromedical evacuation or rescue operations aboard helicopter and propeller aircraft or jet aircraft. Hypersonic Aircraft.
Basic Life Support is a level of medical care which is used for victims of life-threatening illnesses or injuries until they can be given full medical care at a hospital. It can be provided by trained medical personnel, including emergency medical technicians, paramedics, and by qualified bystanders. (BLS)
Advanced Cardiac Life Support or advanced cardiovascular life support (ACLS) refers to a set of clinical interventions for the urgent treatment of cardiac arrest, stroke and other life-threatening medical emergencies, as well as the knowledge and skills to deploy those interventions. Outside North America, Advanced Life Support is used.
Pediatric Advanced Life Support or PALS, is a 2-day (with an additional self study day) American Heart Association training program. The goal of the course is to aid the pediatric healthcare provider in developing the knowledge and skills necessary to efficiently and effectively manage critically ill infants and children, resulting in improved outcomes. Professional healthcare providers use PALS during the stabilization and transportation phases of a pediatric emergency, in or out of hospital.
Mobile Army Surgical Hospital or MASH, refers to a United States Army medical unit serving as a fully functional hospital in a combat area of operations.
Combat Medic are military personnel who have been trained to at least an EMT level (16 week course in the U.S. Army), and are responsible for providing first aid and frontline trauma care on the battlefield. They are also responsible for providing continuing medical care in the absence of a readily available physician, including care for disease and battle injuries. Combat medics are normally co-located with the combat troops they serve in order to easily move with the troops and monitor ongoing health.
Triage is the process of determining the priority of patients' treatments based on the severity of their condition. This rations patient treatment efficiently when resources are insufficient for all to be treated immediately. Those who are likely to live, regardless of what care they receive; Those who are unlikely to live, regardless of what care they receive; Those for whom immediate care might make a positive difference in outcome.
Emergency Medical Services are a type of emergency service dedicated to providing out-of-hospital acute medical care, transport to definitive care, and other medical transport to patients with illnesses and injuries which prevent the patient from transporting themselves. CDC - RT.
Emergency Services are organizations which ensure public safety and health by addressing different emergencies. Some of these agencies exist solely for addressing certain types of emergencies whilst others deal with ad hoc emergencies as part of their normal responsibilities. Many of these agencies engage in community awareness and prevention programs to help the public avoid, detect, and report emergencies effectively. The availability of emergency services depends very heavily on location, and may in some cases also rely on the recipient giving payment or holding suitable insurance or other surety for receiving the service.
Medical Emergency is an acute injury or illness that poses an immediate risk to a person's life or long-term health, sometimes referred to as a situation risking "life or limb". These emergencies may require assistance from another person, who should ideally be suitably qualified to do so, although some of these emergencies such as cardiovascular (heart), respiratory, and gastrointestinal cannot be dealt with by the victim themselves. Dependent on the severity of the emergency, and the quality of any treatment given, it may require the involvement of multiple levels of care, from first aiders through emergency medical technicians, paramedics, emergency physicians and anesthesiologists. Any response to an emergency medical situation will depend strongly on the situation, the patient involved, and availability of resources to help them. It will also vary depending on whether the emergency occurs whilst in hospital under medical care, or outside medical care (for instance, in the street or alone at home).
Intensive Care Unit cater to patients with severe or life-threatening illnesses and injuries, which require constant care, close supervision from life support equipment and medication in order to ensure normal bodily functions. They are staffed by highly trained physicians, nurses and respiratory therapists who specialize in caring for critically ill patients. ICUs are also distinguished from general hospital wards by a higher staff-to-patient ratio and to access to advanced medical resources and equipment that is not routinely available elsewhere. Common conditions that are treated within ICUs include acute (or adult) respiratory distress syndrome, hypertension, metastases and other life-threatening conditions. Patients may be referred directly from an emergency department or from a ward if they rapidly deteriorate, or immediately after surgery if the surgery is very invasive and the patient is at high risk of complications,
AEMT-CC is an Emergency Medical Services (EMS) certification unique to New York.
Drowning: Unconsciopus, pale or blue skin. CPR and mouth to mouth resuscitation. Be extremely careful when moving victims head or neck.
Hypothermia (cold)
The environment is cold. The person may be shivering, pale and cold to touch. They may also be disorientated. Many instances of hypothermia occur inside when there is cold weather and a lack of heating. Warm the person, giving constant reassurance until help arrives. You can warm them by wrapping them in a blanket and giving warm drinks and high-energy foods, such as chocolate. Breathing.
Seizures - Epilepsy: Do not restrain them but use a blanket or clothing to protect their head from injury. Let the seizure run its normal course. After the seizure, help the person to rest on their side with their head tilted back.
Convulsions: Strong jerking movements, stiff body, difficulty breathing, bluish face, eyes rolled back, gritting of teeth, frothy mouth. Loosen clothing and cover body.
Asthma Attack: Help the person sit in a comfortable position and take their medication. When someone has an asthma attack, the muscles in the airways narrow, making it difficult for them to breathe. Using an inhaler relaxes the muscles, allowing the air passages to expand and ease the person’s breathing. A mild attack should ease within a few minutes. If it doesn’t, or the inhaler has no effect, call 999.
Fainting: clammy skin, dizziness, shallow breathing, sweating, temporary unconsciousness. Place in Supine position with legs higher than body. Loosen clothing. Apply cold cloths to face. Fainting occurs when the blood supply to your brain is momentarily inadequate, causing you to lose consciousness. This loss of consciousness is usually brief. Fainting can have no medical significance, or the cause can be a serious disorder. Therefore, treat loss of consciousness as a medical emergency until the signs and symptoms are relieved and the cause is known. Discuss recurrent fainting spells with your doctor. If you feel faint Lie down or sit down. To reduce the chance of fainting again, don't get up too quickly. Place your head between your knees if you sit down. If someone else faints Position the person on his or her back. If the person is breathing, restore blood flow to the brain by raising the person's legs above heart level — about 12 inches (30 centimeters) — if possible. Loosen belts, collars or other constrictive clothing. To reduce the chance of fainting again, don't get the person up too quickly. If the person doesn't regain consciousness within one minute, call 911 or your local emergency number. Check the person's airway to be sure it's clear. Watch for vomiting. Check for signs of circulation (breathing, coughing or movement). If absent, begin CPR. Call 911 or your local emergency number. Continue CPR until help arrives or the person responds and begins to breathe. If the person was injured in a fall associated with a faint, treat any bumps, bruises or cuts appropriately. Control bleeding with direct pressure. Breathing.
Heat Exhaustion: High Temperature. pale and clammy skin, or hot and flushed skin. headache and weakness. Possible nausea. Apply cold cloths to skin. Give balanced salt solution. Call doctor if person is Confused. Hyperthermia.
Diabetes: Give them something sweet to eat or a non-diet drink. In diabetic emergencies, blood sugar levels can become too low; this can cause people to collapse. Giving them something sugary will help raise their blood sugar levels and improve their bodily function. Avoid giving them a diet drink, as it won’t have any sugar in it and will not help them.
Distressed: Show you are listening and calmly ask them how you can help You must try to establish trust by showing them respect. Be considerate of what is going on around them and what they need. Remember that they may have difficulty letting you know what they need. For example, they may not speak English very well or be able to hear you. Trauma.
Shock: Pale and weak. Clammy skin. Perspiration on upper lip or forehead. Pulse rate and breathing rate high. Lay down and raise feet higher then body. Give no fluid if unconscious. Abdominal pain call ambulance.
Meningitis: The person may have flu-like symptoms, a headache and a high temperature. The person may also complain of a stiff neck and be sensitive to light. At a later stage a rash may form (that does not disappear when a glass is pressed against it). Other symptoms include cold hands and feet, joint pain, drowsiness and vomiting. A person with meningitis can have one or more symptoms, and some symptoms occur later on as the infection develops. Do not wait for all the symptoms to appear. A person with meningitis can deteriorate very quickly. It is potentially very serious and needs immediate attention. If they have a fever, you can use cold drinks to cool the person.
Burns
Cool the burn under cold running water for at least ten minutes. Cooling the burn will reduce pain, swelling and the risk of scarring. The faster and longer a burn is cooled, the less the impact of the injury. After the burn has been cooled, cover it with cling film or a clean plastic bag. This helps prevent infection by keeping the area clean. It’s an ideal covering because it doesn’t stick to the burn and reduces pain by keeping air from the skin’s surface. The burn may need urgent medical treatment. If you’re in any doubt, seek medical advice and always call 999 if a child has been burned.
Minor burns: Cool the burn to help soothe the pain. Hold the burned area under cool (not cold) running water for 10 to 15 minutes or until the pain eases. Or apply a clean towel dampened with cool tap water. Remove rings or other tight items from the burned area. Try to do this quickly and gently, before the area swells. Don't break small blisters (no bigger than your little fingernail). If blisters break, gently clean the area with mild soap and water, apply an antibiotic ointment, and cover it with a nonstick gauze bandage. Apply moisturizer or aloe vera lotion or gel, which may provide relief in some cases. If needed, take an over-the-counter pain reliever, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others). Consider a tetanus shot. Make sure that your tetanus booster is up to date. Doctors recommend people get a tetanus shot at least every 10 years. See your doctor if you develop large blisters. Large blisters are best removed, as they rarely will remain intact on their own. Also seek medical help if the burn covers a large area of the body or if you notice signs of infection, such as oozing from the wound and increased pain, redness and swelling.
Major burns: Call 911 or emergency medical help for major burns. Until an emergency unit arrives, take these actions: Protect the burned person from further harm. If you can do so safely, make sure the person you're helping is not in contact with smoldering materials or exposed to smoke or heat. But don't remove burned clothing stuck to the skin. Check for signs of circulation. Look for breathing, coughing or movement. Begin CPR if needed. Remove jewelry, belts and other restrictive items, especially from around burned areas and the neck. Burned areas swell rapidly. Don't immerse large severe burns in cold water. Doing so could cause a serious loss of body heat (hypothermia) or a drop in blood pressure and decreased blood flow (shock). Elevate the burned area. Raise the wound above heart level, if possible. Cover the area of the burn. Use a cool, moist, bandage or a clean cloth. Is it a minor burn or a major burn? If it's not clear what level of care is needed, try to judge the extent of tissue damage, based on the following burn categories:
1st-degree burn: A first-degree burn is the least serious type, involving only the outer layer of skin. It may cause: Redness, Swelling, Pain. You can usually treat a first-degree burn as a minor burn. If it involves much of the hands, feet, face, groin, buttocks or a major joint, seek emergency medical attention.
2nd-degree burn: A second-degree burn is more serious. It may cause: Red, white or splotchy skin, Swelling, Pain, Blisters. If the second-degree burn is no larger than 3 inches (7.6 centimeters) in diameter, treat it as a minor burn. If the burned area is larger or covers the hands, feet, face, groin, buttocks or a major joint, treat it as a major burn and get medical help immediately.
3rd-degree burns:The most serious burns involve all layers of the skin and underlying fat. Muscle and even bone may be affected. Burned areas may be charred black or white. The person may experience: Difficulty breathing, Carbon monoxide poisoning, Other toxic effects, if smoke inhalation also occurred.
First Aid Tips : How to Treat Second and Third-Degree Burns (youtube)
Skin Cell Gun - Film
Chemical Burns: Chemical burns can be caused by many substances, such as strong acids, drain cleaners (lye), paint thinner and gasoline. Usually, you are aware of the burn and its cause. But sometimes you may not immediately recognize a burn caused by a milder chemical. As with some sunburns, the pain and redness may develop hours after the exposure. If you have an immediately recognized chemical burn. Remove the chemical causing the burn while protecting yourself. For dry chemicals, brush off any remaining material. Wear gloves or use a towel or other suitable object, such as a brush. Remove contaminated clothing or jewelry to prevent further burning. Rinse the burn immediately. Run a gentle, steady stream of cool tap water over the burn for 10 or more minutes. A shower may be an effective way to do this. Always protect your eyes. Loosely apply a bandage or gauze. If needed, take an over-the-counter pain reliever, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others). Consider a tetanus shot. Make sure that your tetanus booster is up to date. Doctors recommend people get a tetanus shot at least every 10 years. If you have a possible chemical burn Make sure that any contaminated clothing or jewelry is no longer in contact with your skin. Rinse the burn if you think some of the chemical is still on your skin. Loosely apply a bandage or gauze. If needed, take an over-the-counter pain reliever, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others). Consider a tetanus shot. Make sure that your tetanus booster is up to date. When to seek emergency care: TThe person shows signs of shock, such as fainting, pale complexion or very shallow breathing. The chemical burn penetrated through the first layer of skin and the burn covers an area more than 3 inches (about 8 centimeters) in diameter. The chemical burn encircles a limb or involves the eyes, hands, feet, face, groin or buttocks, or a major joint. If you're unsure whether a substance is toxic, call Poison Help at 800-222-1222 in the United States. If you seek emergency medical help, take the chemical container or the name of the chemical with you to the emergency department.
Electrical burns: Electrical burns may be caused by a number of sources of electricity, such as lightning, stun guns and contact with household current. You may treat minor electrical burns as you would other minor burns. When to contact your doctor. A person who has been injured by contact with electricity should be seen by a doctor. Sometimes an electrical injury can cause damage to internal tissues, usually in an arm or a leg. The damage may be worse than one would expect from the burn on the skin.
Caution: Don't touch the injured person if he or she is still in contact with the electrical current. Call 911 or your local emergency number if the source of the burn is a high-voltage wire or lightning. Don't get near high-voltage wires until the power is turned off. Overhead power lines usually aren't insulated. Stay at least 20 feet (about 6 meters) away — farther if wires are jumping and sparking. Don't move a person with an electrical injury unless the person is in immediate danger.
When to seek emergency care: Call 911 or your local emergency number if the injured person experiences: Severe burns, Confusion, Difficulty breathing, Heart rhythm problems (arrhythmias), Cardiac arrest, Muscle pain and contractions, Seizures, Loss of consciousness. Take these actions immediately while waiting for medical help: Turn off the source of electricity if possible. If not, move the source away from both you and the injured person using a dry, nonconducting object made of cardboard, plastic or wood. Begin CPR if the person shows no signs of circulation, such as breathing, coughing or movement. Try to prevent the injured person from becoming chilled. Apply a bandage. Cover any burned areas with a sterile gauze bandage, if available, or a clean cloth. Don't use a blanket or towel, because loose fibers can stick to the burns
Electrical Shock: The danger from an electrical shock depends on the type of current, how high the voltage is, how the current traveled through the body, the person's overall health and how quickly the person is treated. An electrical shock may cause burns, or it may leave no visible mark on the skin. In either case, an electrical current passing through the body can cause internal damage, cardiac arrest or other injury. Under certain circumstances, even a small amount of electricity can be fatal. A person who has been injured by contact with electricity should be seen by a doctor. Caution: Don't touch the injured person if he or she is still in contact with the electrical current. Call 911 or your local emergency number if the source of the burn is a high-voltage wire or lightning. Don't get near high-voltage wires until the power is turned off. Overhead power lines usually aren't insulated. Stay at least 20 feet (about 6 meters) away — farther if wires are jumping and sparking. Don't move a person with an electrical injury unless he or she is in immediate danger. When to seek emergency care: Call 911 or your local emergency number if the injured person experiences: Severe burns, Confusion, Difficulty breathing, Heart rhythm problems (arrhythmias) Cardiac arrest, Muscle pain and contractions, Seizures, Loss of consciousness. Take these actions immediately while waiting for medical help: Turn off the source of electricity, if possible. If not, move the source away from you and the person, using a dry, nonconducting object made of cardboard, plastic or wood. Begin CPR if the person shows no signs of circulation, such as breathing, coughing or movement. Try to prevent the injured person from becoming chilled. Apply a bandage. Cover any burned areas with a sterile gauze bandage, if available, or a clean cloth. Don't use a blanket or towel, because loose fibers can stick to the burns.
Sun Burn: Redness. Mild swelling and pain. Possible blisters. Apply cold cream or cold towels. Fever, chills and sickness may accompany a severe burn and your Doctor should be called. Protect person from Sun. Take a cool bath or shower, which may be soothing. Or apply a clean towel dampened with cool tap water. Apply moisturizer, aloe vera lotion or gel, or low-dose hydrocortisone cream, which may provide relief in some cases. Don't break small blisters (no bigger than your little fingernail). If blisters break, gently clean the area with mild soap and water, apply an antibiotic ointment, and cover it with a nonstick gauze bandage. UV Index - Skin Cancer
Blisters: If a blister isn't too painful, try to keep it intact. Unbroken skin over a blister may provide a natural barrier to bacteria and decreases the risk of infection. Cover it with an adhesive bandage. If you're allergic to the adhesive used in some tape, use paper tape. Seek medical care if the blister is painful or prevents you from walking or using one of your hands. Consider taking the following self-care measures if medical help is not available. How to drain a blister: To relieve blister-related pain, drain the fluid while leaving the overlying skin intact. Here's how: Wash your hands and the blister with soap and warm water. Swab the blister with iodine. Sterilize a clean, sharp needle by wiping it with rubbing alcohol. Use the needle to puncture the blister. Aim for several spots near the blister's edge. Let the fluid drain, but leave the overlying skin in place. Apply an ointment (Vaseline, Plastibase, other) to the blister and cover it with a nonstick gauze bandage. If a rash appears, stop using the ointment. Change the dressing every day. Apply more ointment and a bandage. Blister prevention: To prevent friction blisters on your feet, wear shoes that fit well. It also helps to use moisture-wicking socks. Try the various socks, shoes and insoles that are designed specifically to help reduce blistering. You might also try attaching moleskin to the inside of your shoe where it might rub or dusting the inside of your socks with talcum powder. Gloves help prevent blisters on your hands.
Blister is a small pocket of body fluid (lymph, serum, plasma, blood, or pus) within the upper layers of the skin, typically caused by forceful rubbing (friction), burning, freezing, chemical exposure or infection. Most blisters are filled with a clear fluid, either serum or plasma. However, blisters can be filled with blood (known as "blood blisters") or with pus (for instance, if they become infected).
Skin Grafting is a type of graft surgery involving the transplantation of skin. The transplanted tissue is called a skin graft. Skin grafting is often used to treat: Extensive wounding or trauma, Burns, Areas of extensive skin loss due to infection such as necrotizing fasciitis or purpura fulminans, Specific surgeries that may require skin grafts for healing to occur - most commonly removal of skin cancers.



